Autoimmune hepatitis
Conditions
Overview
Autoimmune hepatitis is a liver disease that happens when the body's immune system attacks the liver. This can cause swelling, irritation and damage to the liver. The exact cause of autoimmune hepatitis is unclear, but genetic and environmental factors appear to interact over time to trigger the disease.
Untreated autoimmune hepatitis can lead to scarring of the liver, called cirrhosis. It can also eventually lead to liver failure. When diagnosed and treated early, however, autoimmune hepatitis often can be controlled with medicines that suppress the immune system.
A liver transplant may be an option when autoimmune hepatitis doesn't respond to medicines or liver disease becomes advanced.
Symptoms
Symptoms of autoimmune hepatitis vary from person to person and may come on suddenly. Some people have few, if any, recognized problems in the early stages of the disease, whereas others experience symptoms that may include:
- Fatigue.
- Belly discomfort.
- Yellowing of the skin and whites of the eyes, called jaundice. Depending on skin color, this change may be harder or easier to see.
- An enlarged liver.
- Irregular blood vessels on the skin, called spider angiomas.
- Skin rash.
- Joint pain.
- Loss of menstrual periods.
When to see a doctor
Make an appointment with a healthcare professional if you have any symptoms that worry you.
Causes
Autoimmune hepatitis occurs when the body's immune system, which usually attacks viruses, bacteria and other causes of disease, instead targets the liver. This attack on the liver can lead to long-lasting inflammation and serious damage to liver cells. Just why the body turns against itself is unclear, but researchers think autoimmune hepatitis could be caused by the interaction of genes controlling immune system function and exposure to viruses or medicines.
Types of autoimmune hepatitis
Experts have identified two main forms of autoimmune hepatitis.
- Type 1 autoimmune hepatitis. This is the most common type of the disease. It can occur at any age. About half the people with type 1 autoimmune hepatitis have other autoimmune disorders, such as celiac disease, rheumatoid arthritis or ulcerative colitis.
- Type 2 autoimmune hepatitis. Although adults can develop type 2 autoimmune hepatitis, it's most common in children and young people. Other autoimmune diseases may accompany this type of autoimmune hepatitis.
Risk factors
Factors that may increase your risk of autoimmune hepatitis include:
- Being female. Although both males and females can develop autoimmune hepatitis, the disease is most common in females.
- Genetics. Evidence suggests that a predisposition to autoimmune hepatitis may run in families.
- Having an autoimmune disease. People who already have an autoimmune disease, such as celiac disease, rheumatoid arthritis or hyperthyroidism (Graves' disease or Hashimoto thyroiditis), may be more likely to develop autoimmune hepatitis.
Complications
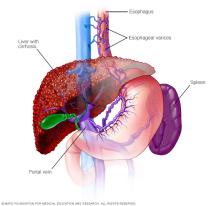
Autoimmune hepatitis that goes untreated can cause permanent scarring of the liver tissue, known as cirrhosis. Complications of cirrhosis include:
-
Enlarged veins in the esophagus, called esophageal varices. The portal vein carries blood from the intestine to the liver. When circulation through the portal vein is blocked, blood may back up into other blood vessels, mainly those in the stomach and esophagus.
These blood vessels have thin walls. And because they become filled with more blood than they're meant to carry, they're likely to bleed. Massive bleeding in the esophagus or stomach from these blood vessels is a life-threatening emergency that needs immediate medical care.
- Fluid in the abdomen, called ascites (uh-SY-teez). Liver disease can cause large amounts of fluid to build up in the belly. Ascites can be uncomfortable and may interfere with breathing. It's usually a sign of advanced cirrhosis.
- Liver failure. Liver failure happens when extensive damage to liver cells makes it not possible for the liver to function well. At this point, a liver transplant is needed.
- Liver cancer. People with cirrhosis have an increased risk of liver cancer.
Diagnosis

Tests and procedures used to diagnose autoimmune hepatitis include:
- Blood tests. Testing a sample of blood for antibodies can distinguish autoimmune hepatitis from viral hepatitis and other conditions with similar symptoms. Antibody tests also help pinpoint the type of autoimmune hepatitis you have.
- Liver biopsy. A sample of liver tissue may be taken to confirm the diagnosis and to determine the degree and type of liver damage. During the biopsy procedure, a thin needle is passed into the liver through a small cut in the skin. The needle is used to take a small sample of liver tissue. The sample is then sent to a laboratory for testing.
Treatment
The goal of treatment for autoimmune hepatitis is to slow or stop the immune system attack on the liver. This may help increase the time before the disease gets worse. To meet this goal, you'll likely need medicines that lower immune system activity. The first treatment is usually prednisone. A second medicine, azathioprine (Azasan, Imuran), may be recommended in addition to prednisone.
Prednisone, especially when taken long term, can cause a wide range of serious side effects, including diabetes, weakened or broken bones, high blood pressure, cataracts, glaucoma, and weight gain.
Healthcare professionals typically prescribe prednisone at a high dose for about the first month of treatment. Then, to reduce the risk of side effects, they gradually reduce the dose over the next several months until reaching the lowest possible dose that controls the disease. Adding azathioprine also helps you avoid prednisone side effects.
Although you may experience remission a few years after starting treatment, the disease often returns if the drug is discontinued. Depending on your situation, you may need lifelong treatment.
Liver transplant
When medicines don't stop the disease from getting worse or you get scarring that can't be reversed — called cirrhosis — or liver failure, the remaining option is a liver transplant.
During a liver transplant, your diseased liver is removed and replaced with a healthy liver from a donor. Liver transplants most often use livers from deceased organ donors. In some cases, a living-donor liver transplant can be used. During a living-donor liver transplant, you receive only a part of a healthy liver from a living donor. Both livers begin regenerating new cells almost right away.
Preparing for an appointment
If you have any symptoms that worry you, start by making an appointment with someone on your primary healthcare team. If your care team suspects that you may have autoimmune hepatitis, you may be referred to a specialist in liver diseases. This type of specialist is called a hepatologist.
Because appointments can be brief and there's often a lot to discuss, it's a good idea to be prepared for your appointment. Here's some information to help you get ready and know what to expect.
What you can do
- Be aware of any pre-appointment restrictions. At the time you make the appointment, be sure to ask if there's anything you need to do in advance, such as restrict your diet.
- Write down any symptoms you're experiencing, including any that may seem unrelated to the reason for which you scheduled the appointment.
- Write down key personal information, including any major stresses or recent life changes.
- Make a list of all medications, vitamins or supplements that you're taking.
- Take a family member or friend along to help you remember everything that was discussed.
- Write down questions to ask your care team.
For autoimmune hepatitis, some basic questions to ask include:
- What's the most likely cause of my symptoms?
- Are there any other possible causes?
- What tests do I need to confirm that I have autoimmune hepatitis?
- How severe is the damage to my liver?
- Is my condition likely temporary or chronic?
- What are my treatment options?
- Can treatment cure my autoimmune hepatitis?
- What are the potential side effects of each treatment option?
- How might treatment for autoimmune hepatitis affect the management of my other medical conditions?
- Could any of my medicines or habits cause my liver problems or make my liver problems worse?
- Are there any dietary restrictions that I need to follow?
- Should I see a specialist?
- Is there a generic alternative to the medicine you're prescribing me?
- Are there any brochures or other printed material that I can take with me? What websites do you recommend?
- How often will I need follow-up visits?
What to expect from your doctor
You'll likely be asked a few questions during the appointment. Being ready to answer them may reserve time to go over any points you want to spend more time on. You may be asked:
- When did you first begin experiencing symptoms?
- Have your symptoms been continuous or occasional?
- How severe are your symptoms?
- Does anything seem to improve or worsen your symptoms?
- Are you taking any medicines or treatments for your symptoms?
- Do you have a family history of liver disease?
© 1998-2026 Mayo Foundation for Medical Education and Research(MFMER). All rights reserved. Terms of Use
