Hilar cholangiocarcinoma
Conditions
Overview
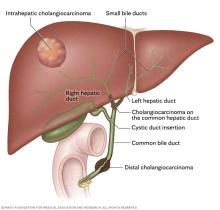
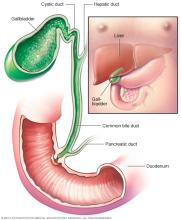
Hilar (HY-lur) cholangiocarcinoma, also called perihilar (per-e-HY-lur) cholangiocarcinoma or Klatskin tumor, is a type of cancer that starts as a growth of cells that are not typical in the bile ducts. Bile ducts are slender tubes that carry the digestive fluid called bile from the liver to the small intestine.
Cholangiocarcinoma is the medical term for bile duct cancer, and it is classified by location into three types. Hilar cholangiocarcinoma happens where the right and left bile ducts that lead out of the liver join to form the common hepatic duct.
Other bile duct cancers include intrahepatic cholangiocarcinoma, which starts inside the liver, and distal cholangiocarcinoma, which occurs lower in the bile duct near the pancreas. Hilar cholangiocarcinoma is the most common type of bile duct cancer, but it is still a rare form of cancer overall. Common symptoms include yellowing of the skin and the whites of the eyes, weight loss, stomach pain, and itching.
Treatment for hilar cholangiocarcinoma may include surgery to remove the cancer or a combination treatment plan that includes radiation therapy followed by a liver transplant. Surgery is often complex and may require taking out part of the liver along with the affected bile ducts. Other treatments may include chemotherapy, radiation therapy, immunotherapy and targeted therapy.
Symptoms
Hilar cholangiocarcinoma may not cause symptoms at first. Symptoms typically happen when the cancer grows and blocks the bile ducts, preventing bile from draining from the liver into the intestine. Signs and symptoms of hilar cholangiocarcinoma may include:
- Yellowing of the skin and the whites of the eyes, known as jaundice.
- Itching.
- Dark urine.
- Clay-colored stools.
- Stomach pain.
- Fatigue.
- Weight loss.
When to see a doctor
Make an appointment with a doctor or other healthcare professional if you have any symptoms that worry you.
Causes
It's not clear what causes most hilar cholangiocarcinomas, but the cancer is often linked to long-term inflammation or injury of the bile ducts. This cancer starts in the bile ducts that connect the liver to the small intestine. Conditions such as primary sclerosing cholangitis, bile duct cysts or stones, liver fluke infection, and long-lasting liver disease increase the risk of developing this cancer.
Hilar cholangiocarcinoma, also called perihilar cholangiocarcinoma or Klatskin tumor, develops when cells in a bile duct get changes in their DNA. A cell's DNA contains the instructions that tell the cell how to grow and when to die. In healthy cells, these instructions keep growth under control. In cancer cells, DNA changes give faulty instructions that tell the cells to grow and divide too quickly and to keep living when typical cells would die.
The buildup of these cells can form a tumor in the bile ducts. Long-term inflammation or injury to the bile ducts, such as from primary sclerosing cholangitis or bile duct cysts, can increase the chance of having these DNA changes.
The cancer cells form a mass called a tumor. The tumor can grow to invade and destroy healthy body tissue. In time, cancer cells can break away and spread to other parts of the body. When cancer spreads, it's called metastatic cancer.
Risk factors
Factors that may increase the risk of hilar cholangiocarcinoma include:
- Primary sclerosing cholangitis. Primary sclerosing cholangitis causes inflammation, hardening and scarring of the bile ducts that can lead to cancer.
- Older age. Hilar cholangiocarcinoma happens most often in adults over age 50. However, it can develop at a younger age in people who have primary sclerosing cholangitis.
- Inflammatory bowel disease. People who have ongoing inflammation of the digestive tract have an increased risk of hilar cholangiocarcinoma.
- Liver cirrhosis. Liver cirrhosis causes scarring of the liver that increases the risk of hilar cholangiocarcinoma.
- Bile duct cysts. Bile duct cysts cause bile ducts to change and get larger. Having bile duct cysts, also called Caroli disease, increases the risk of hilar cholangiocarcinoma.
- Gallbladder conditions. Ongoing inflammation of the gallbladder, called cholecystitis, increases the risk of hilar cholangiocarcinoma. People who get gallstones also are at an increased risk.
- Liver parasites. In areas of Southeast Asia, hilar cholangiocarcinoma is linked to liver flukes. These are parasites that can infect humans. Liver fluke infection can happen from eating raw or undercooked fish.
Complications
Hilar cholangiocarcinoma can lead to several complications, mostly because the tumor blocks the flow of bile from the liver. This blockage can cause infections, liver damage, and other issues that affect digestion and overall health, including:
- Infection in the bile ducts, called cholangitis. When bile can't drain properly, bacteria can grow inside the ducts, leading to infection, fever and chills.
- Liver damage and liver failure. Long-term bile blockage can scar and damage the liver, causing it to not function properly.
- Malnutrition and vitamin deficiency. Because bile helps digest fats, blockage can cause poor absorption of nutrients and vitamins, leading to weight loss and weakness.
- Portal hypertension. Tumor growth or scarring can increase pressure in the veins of the liver, which may cause swelling of the abdomen or enlarged veins in the esophagus.
- Cancer spread, called metastasis. The liver and nearby lymph nodes are common sites of metastases for hilar cholangiocarcinoma. Spread to distant sites, such as the lungs, brain and bones, is not common.
Diagnosis
Diagnosing hilar cholangiocarcinoma, also called perihilar cholangiocarcinoma or Klatskin tumor, often begins with a physical exam. Your healthcare professional also will likely ask about your health history. You may have imaging tests and blood tests. A sample of tissue may be taken for lab testing.
Imaging tests
Imaging tests make pictures of the inside of the body. They help your healthcare team see the location, size and spread of a hilar cholangiocarcinoma.
- Ultrasound is often the first test. It can show whether the bile ducts are blocked or enlarged.
- CT scans take detailed pictures of the liver and bile ducts, especially the blood vessels going into the liver. They help show if the cancer has spread or can be taken out with surgery.
- MRI gives even more detailed pictures of the liver and bile ducts.
- Magnetic resonance cholangiopancreatography (MRCP) is a special type of MRI that makes clear images of the bile ducts, liver, gallbladder and pancreas to help find the exact spot of the blockage or tumor.
- Endoscopic retrograde cholangiopancreatography (ERCP) and percutaneous transhepatic cholangiography (PTC). Many people with hilar cholangiocarcinoma develop jaundice because the tumor blocks the bile ducts. When imaging shows a blockage, procedures such as ERCP or PTC may be used to look at the bile ducts, obtain tissue samples and define the extent of the tumor. These procedures can also help relieve the blockage by placing stents or drainage tubes to allow bile to flow, which often improves symptoms and helps prevent infection.
Liver function tests
Blood tests to measure your liver function can give your healthcare team clues about what's causing your symptoms.
Tumor marker tests
A tumor marker test looks for substances called tumor markers. These markers are often made by cancer cells or healthy cells in response to cancer. Checking the level of the tumor markers in your blood may give your healthcare team more clues about your diagnosis.
Tumor markers for hilar cholangiocarcinoma include carbohydrate antigen 19-9, also called CA 19-9, and carcinoembryonic antigen, also called CEA. These are proteins that are overproduced by cholangiocarcinoma cells. Then levels of these tumor markers are high, it may mean a more advanced cancer.
Having high levels of CA 19-9 and CEA in your blood doesn't always mean you have hilar cholangiocarcinoma. This also can happen with other bile duct conditions, such as bile duct inflammation and obstruction.
Biopsy
A biopsy is a procedure to remove a sample of tissue for testing in a lab. To get a sample of tissue from a hilar cholangiocarcinoma, a healthcare professional might use a procedure called endoscopic retrograde cholangiopancreatography (ERCP). During this procedure, a health professional puts a thin tube with a camera down the throat. The tube, called an endoscope, goes through the stomach and into the small intestine to get to the bile duct. The endoscope is used to put contrast material into the bile duct to help it show more clearly on X-rays. The X-ray images help guide the endoscope to the right place. A brush tool can extend from the endoscope to collect cells from the cancer.
Treatment
Treatment for hilar cholangiocarcinoma depends on the location and extent of the cancer. Surgery is the main treatment and offers the only chance to cure the disease if all the cancer can be taken out. For some people, a liver transplant also may be an option.
If surgery or transplant is not possible, other treatments are used to control the cancer and ease symptoms. These may include radiation therapy, radiofrequency ablation and medicines. Medicines used to treat hilar cholangiocarcinoma include chemotherapy, targeted therapy and immunotherapy.
Your healthcare team considers many factors when creating a treatment plan. These factors may include your overall health, the type and stage of your cancer, and your preferences.
Surgery
The goal of surgery for hilar cholangiocarcinoma is to take out all of the cancer. But it may not be an option for everyone. This cancer grows near many important structures, which can make surgery difficult. Less than half of people can have surgery when they are first diagnosed because many already have cancer that has spread too far.
When surgery is possible, options may include:
- Surgery to remove the cancer. Removing the cancer often includes taking out and rebuilding part of the bile duct and nearby structures, such as the surrounding ducts and parts of the liver and gallbladder.
- Removing nearby lymph nodes. Lymph nodes may be taken out to be tested for cancer. Removing cancerous lymph nodes may help prevent the spread of the cancer.
- Liver transplant. Sometimes, using surgery to take out just the cancer is not possible. If the cancer can't be removed with surgery but has not spread outside the liver, radiation therapy can be combined with a liver transplant. After radiation therapy, a surgeon removes the cancer and all of the liver. Then the surgeon puts a healthy liver from a donor into the body.
- Biliary drainage. Biliary drainage uses a procedure to restore the flow of bile if cancer blocks a bile duct. This procedure might involve placing a thin tube into the bile duct to drain the bile. Sometimes a surgeon does a bypass surgery to route the bile duct around the cancer. Another kind of procedure might involve placing stents to hold open a bile duct being collapsed by cancer. Biliary drainage helps relieve symptoms of hilar cholangiocarcinoma.
Radiation therapy
Radiation therapy treats cancer with powerful energy beams. The energy can come from X-rays, protons or other sources. During radiation therapy, you lie on a table while a machine moves around you. The machine directs radiation to precise points on your body.
For hilar cholangiocarcinoma, radiation therapy is sometimes combined with chemotherapy to kill cancer cells that remain after surgery. Radiation therapy also may be combined with chemotherapy to treat cancer that has spread to the lymph nodes.
Sometimes the healthcare team uses other procedures to place radiation close to the cancer. One way to do this is with a procedure called radioembolization. It involves putting small beads that hold radiation into a blood vessel that leads to the cancer. The beads travel through the blood vessel and block the blood supply to the cancer. The beads give off radiation directly to the cancer.
Chemotherapy
Chemotherapy treats cancer with strong medicines. Many chemotherapy medicines exist. Most chemotherapy medicines are given through a vein. Some come in pill form.
For hilar cholangiocarcinoma, chemotherapy may be used after surgery to kill any remaining cancer cells. For those with advanced cancer that can't be taken out with surgery, chemotherapy may be an option to slow the growth of the cancer.
Chemotherapy is sometimes combined with radiation therapy after surgery to kill any remaining cancer cells. Chemotherapy also may be combined with radiation to treat cancer that has spread to the lymph nodes.
Targeted therapy
Targeted therapy for cancer is a treatment that uses medicines that attack specific chemicals in the cancer cells. By blocking these chemicals, targeted treatments can cause cancer cells to die. For those with advanced hilar cholangiocarcinoma that can't be taken out with surgery, targeted therapy may be an option. Some cancer cells might be tested to see if targeted therapy is likely to work on the cancer.
Immunotherapy
Immunotherapy for cancer is a treatment with medicine that helps the body's immune system kill cancer cells. The immune system fights off diseases by attacking germs and other cells, such as cancer cells, that shouldn't be in the body. Cancer cells survive by hiding from the immune system. Immunotherapy helps the immune system cells find and kill the cancer cells. For those with advanced hilar cholangiocarcinoma that can't be taken out with surgery, immunotherapy may be an option.
Palliative care
Palliative care is a special type of healthcare that helps you feel better when you have a serious illness. If you have cancer, palliative care can help ease pain and other symptoms. A healthcare team that may include doctors, nurses and other specially trained health professionals provides palliative care. The care team's goal is to improve quality of life for you and your family.
Palliative care specialists work with you, your family and your care team. They provide an extra layer of support while you have cancer treatment. You can have palliative care at the same time you're getting strong cancer treatments, such as surgery, chemotherapy, immunotherapy, targeted therapy or radiation therapy.
The use of palliative care with other treatments can help people with cancer feel better and live longer.
Coping and support
With time, you'll find ways to cope with feelings that happen after a cancer diagnosis. Until then, here are some ideas for coping with hilar cholangiocarcinoma.
Learn enough about cancer to make decisions about your care
Ask your healthcare team about your cancer, including your test results, treatment options and, if you want, your prognosis. As you learn more about hilar cholangiocarcinoma, you may become more confident in making treatment decisions.
Keep friends and family close
Keeping your close relationships strong can help you deal with hilar cholangiocarcinoma. Friends and family can provide the practical support you may need, such as helping take care of your home if you're in the hospital. And they can serve as emotional support when you feel overwhelmed by having cancer.
Find someone to talk with
Find someone who is willing to listen to you talk about your hopes and worries. This person may be a friend or family member. The concern and understanding of a counselor, medical social worker, clergy member or cancer support group also may be helpful.
Ask your healthcare team about support groups in your area. Other sources of information include the U.S. National Cancer Institute and the American Cancer Society.
Preparing for an appointment
Make an appointment with a doctor or other healthcare professional if you have any symptoms that worry you.
If your healthcare professional thinks you might have hilar cholangiocarcinoma, you may be referred to a doctor who specializes in diseases of the digestive system, called a gastroenterologist. If you have cancer, you also may be referred to a doctor who specializes in treating cancer, called an oncologist.
Because appointments can be brief, it's a good idea to be prepared. Here's some information to help you get ready.
What you can do
- Be aware of anything you need to do ahead of time. At the time you make the appointment, be sure to ask if there's anything you need to do in advance, such as restrict your diet.
- Write down symptoms you have, including any that may not seem related to the reason for which you scheduled the appointment.
- Write down important personal information, including major stresses or recent life changes.
- Make a list of all medicines, vitamins and supplements you take and the doses.
- Take a family member or friend along. Sometimes it can be hard to remember all the information provided during an appointment. Someone who goes with you may remember something that you missed or forgot.
- Write down questions to ask your healthcare team.
Your time with your healthcare team is limited, so preparing a list of questions can help you make the most of your time together. List your questions from most important to least important in case time runs out. For hilar cholangiocarcinoma, some basic questions to ask include:
- Do I have hilar cholangiocarcinoma?
- What is the stage of my hilar cholangiocarcinoma?
- Has my hilar cholangiocarcinoma spread to other parts of my body?
- Will I need more tests?
- What are the treatment options?
- How much does each treatment increase my chances of a cure or prolong my life?
- What are the potential side effects of each treatment?
- How will each treatment affect my daily life?
- Is there one treatment option you believe is the best?
- What would you recommend to a friend or family member in my situation?
- Should I see a specialist?
- Are there any brochures or other printed material that I can take with me? What websites do you recommend?
- What will determine whether I should plan for a follow-up visit?
Don't hesitate to ask other questions.
What to expect from your doctor
Be prepared to answer questions, such as:
- When did your symptoms begin?
- Do your symptoms happen all the time or do they come and go?
- How bad are your symptoms?
- What, if anything, seems to make your symptoms better?
- What, if anything, appears to worsen your symptoms?
If you're diagnosed with hilar cholangiocarcinoma, also called perihilar cholangiocarcinoma or Klatskin tumor, the next step is to determine where the cancer is and how far it has spread, called the stage. Staging may include imaging tests such as MRI, CT scans, PET scans or X-rays. The images help your healthcare team see the cancer's location and any spread.
How staging works
For hilar cholangiocarcinoma, healthcare professionals often use two different systems to learn about the cancer. Together, these systems help guide treatment and predict outcomes:
- Bismuth-Corlette classification. This system describes the location of the cancer in the bile ducts.
- TNM staging. This system describes how far the cancer has spread.
Bismuth-Corlette classification
The Bismuth-Corlette system divides hilar cholangiocarcinoma into four main types based on how far the cancer extends into the bile ducts:
- Type 1. In type 1, the cancer is below the junction of the right and left hepatic ducts.
- Type 2. In type 2, the cancer reaches the junction but does not extend into the right or left ducts.
- Type 3a. In type 3a, the cancer extends into the right hepatic duct.
- Type 3b. In type 3b, the cancer extends into the left hepatic duct.
- Type 4. In type 4, the cancer involves both the right and left hepatic ducts.
This system helps surgeons decide how much of the bile duct and liver may need to be taken out.
TNM staging
The TNM system is the standard for describing cancer stages. The system looks at three main features:
- T. The size of the primary tumor.
- N. Whether the cancer has spread to nearby lymph nodes.
- M. Whether the cancer has spread to other parts of the body, called metastasis.
Healthcare professionals use these features to assign a stage from 1 to 4.
Hilar cholangiocarcinoma stages
Stage 1
At stage 1, the cancer has grown deeper into the wall of the bile duct but has not spread to nearby lymph nodes or other organs.
It is considered localized, meaning the cancer is confined to the bile duct area and can often be treated with surgery to take out the affected section of the bile duct and nearby tissue.
Stage 2
In stage 2 hilar cholangiocarcinoma, the cancer has grown beyond the wall of the bile duct into nearby fat or liver tissue, but it still has not spread to lymph nodes or distant organs.
Surgery to remove the bile ducts and part of the liver may be done along with removal of nearby lymph nodes to check for hidden spread.
Stage 3
Stage 3 means the cancer has spread to nearby lymph nodes or major blood vessels that supply the liver. The cancer also may cause part of the liver to shrink, called atrophy, on one side. Because of this, surgery becomes more complex and may require major liver resection.
Additional treatments such as chemotherapy or radiation therapy may be used before or after surgery to help control the disease.
Stage 4
In stage 4, the cancer has spread to other organs such as the liver, lungs, distant lymph nodes or the lining of the abdomen, called the peritoneum. This stage also is called metastatic disease.
Surgery is usually not possible. Treatment focuses on systemic therapy such as chemotherapy, targeted therapy or immunotherapy to slow the cancer and ease symptoms.
Hilar cholangiocarcinoma, also called perihilar cholangiocarcinoma or Klatskin tumor, is an aggressive cancer that often grows silently until it blocks the bile ducts. Because many people are diagnosed after the disease has already spread, the overall survival rate remains low.
After surgery
Surgery that completely takes out the cancer, often called R0 resection, is the only treatment that offers a chance for long-term survival. When cancer cells are found at the edges of the removed tissue, called an R1 or R2 resection, the survival rate is lower. Survival also is lower when the cancer has spread to lymph nodes or blood vessels.
If the cancer cannot be taken out
If surgery is not possible, treatment focuses on easing symptoms and slowing the cancer's growth. These therapies are not expected to cure the cancer, but they can help improve quality of life and extend survival.
Treatments often include chemotherapy or immunotherapy. Chemotherapy is usually the first treatment offered, and immunotherapy may be considered depending on the tumor's genetic features. Most people in this situation live between six and 12 months, even with treatment.
After liver transplantation
Some people with small, localized tumors that cannot be removed may be offered liver transplantation at specialized centers. In these people, cancer has not spread to lymph nodes or distant organs and they have shown a good response to chemoradiation before transplantation. For some people, outcomes after transplant can be better than those after surgery, such as for people who also have primary sclerosing cholangitis.
© 1998-2026 Mayo Foundation for Medical Education and Research(MFMER). All rights reserved. Terms of Use
