Interstitial lung disease
Conditions
Overview
Interstitial (in-tur-STISH-ul) lung disease, also called ILD, describes a large group of conditions. Most of these conditions cause inflammation and progressive scarring of lung tissue. As part of this process, lung tissue thickens and stiffens, making it hard for the lungs to expand and fill with air.
At some point, the scarring from interstitial lung disease makes it harder to breathe and get enough oxygen into the bloodstream. Many people with ILD are short of breath with activity and may have a bothersome dry cough.
Interstitial lung disease can have many causes, including long-term exposure to hazardous materials such as asbestos. Some types of autoimmune diseases, such as rheumatoid arthritis, also can cause interstitial lung disease. But the cause isn't known sometimes. ILD can have many causes, so treatment varies.
The disease may get worse slowly or rapidly at a pace that often can't be predicted. Once lung scarring occurs, it generally isn't reversible. Treatment focuses on keeping more scarring from occurring, managing symptoms and making quality of life better. Medicines may slow the damage of interstitial lung disease, but many people never fully use their lungs again. Lung transplant is an option for some people who have ILD.
Symptoms
The main symptoms of interstitial lung disease are:
- Shortness of breath at rest or shortness of breath that worsens with physical activity.
- Dry cough.
When to see a doctor
By the time symptoms appear in certain types of interstitial lung disease, lasting lung damage has already occurred. That's why it's important to see your healthcare professional at the first sign of breathing problems. Many conditions other than ILD can affect your lungs. Getting an early and correct diagnosis is important for proper treatment.
Causes
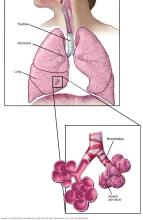
Interstitial lung disease seems to occur when an injury to your lungs causes a healing response that isn't proper. Ordinarily, your body creates just the right amount of tissue to repair damage. But in ILD, the repair process doesn't work properly. Tissue in and around the lungs' air sacs, called alveoli, becomes inflamed, scarred and thickened. This makes it harder for oxygen to pass into your bloodstream.
There are many types of interstitial lung disease. They're generally grouped by known or unknown causes:
- Your work or the environment.
- An underlying systemic condition.
- Certain types of medicines, or radiation.
- No known cause.
Some interstitial lung diseases can be related to smoking.
Your work or the environment
Long-term exposure to some toxins and pollutants can damage your lungs. For example:
- Pneumoconiosis. Pneumoconiosis (noo-moe-koh-nee-O-sis) refers to a type of interstitial lung disease caused by breathing in certain kinds of dust from work or another environment over a long time. Diseases in this group can cause lung scarring and injury over time, leading to shortness of breath and poor ability to take in oxygen. These symptoms can't be reversed. The disease is often named after the exposure type or work role itself. They include such diseases as coal miner's lung, caused by breathing in coal dust, and asbestosis, caused by breathing in asbestos particles. These diseases also include silicosis, caused by breathing in silica dust.
- Hypersensitivity pneumonitis. This lung inflammation is caused by breathing in airborne irritants, often involving the proteins of living things. The most common of these airborne irritants are bird protein, mold or bacteria. Conditions of this type also are often named after the type or source of exposure. For example, pigeon-breeder's or bird-lover's disease involves being exposed to bird protein, and farmer's lung involves being exposed to moldy hay. People with this type of lung inflammation can get better by staying away from the irritant. But this type of lung inflammation also can get worse and lead to more-lasting damage if people continue to breathe in the irritant.
Underlying systemic condition
Certain diseases or conditions may lead to interstitial lung disease. For example:
- Connective tissue diseases. These include autoimmune diseases, such as rheumatoid arthritis, scleroderma and mixed connective tissue disease. These diseases result in an immune response that isn't proper and may cause tissue inflammation and scarring in the body, including in the lungs.
- Sarcoidosis. This is a disease that includes the growth of tiny collections of inflammatory cells called granulomas in any part of your body — most commonly the lungs and lymph nodes. Other commonly affected organs include the eyes, skin, heart, spleen and liver.
Medications, radiation
Certain types of medicines can cause interstitial lung disease in some people. This may or may not be reversible based on the type and length of exposure.
Medicines more commonly associated with ILD are:
- Chemotherapy drugs. Drugs designed to kill cancer cells, such as bleomycin, gemcitabine and immune checkpoint inhibitors, can damage lung tissue.
- Heart medicines. Some drugs used to treat irregular heartbeats, such as amiodarone (Nexterone, Pacerone), may harm lung tissue.
- Some antibiotics. Nitrofurantoin (Macrobid, Macrodantin, others) and daptomycin can cause lung damage.
- Anti-inflammatory drugs. Certain anti-inflammatory drugs, such as methotrexate (Trexall, Xatmep, others) or sulfasalazine (Azulfidine), can damage the lungs.
Radiation directed at the chest during treatments for certain types of cancers — breast and lung cancers, for example — may lead to injury or long-term scarring in some people. How severe the damage is may depend on:
- How much of the lung was exposed to radiation.
- The total amount of radiation given.
- Whether chemotherapy also was used.
- Whether there is underlying lung disease.
No known cause
The list of substances and conditions that can lead to interstitial lung disease is long. Even so, in some people, the cause is never found. Conditions without a known cause are grouped together under the label of idiopathic interstitial pneumonias. For example:
- Idiopathic pulmonary fibrosis, also called IPF. IPF is a typically progressive lung disease that occurs when lung tissue becomes damaged and scarred — what's known as fibrosis. Idiopathic means the cause isn't known. IPF can be seen on imaging and biopsy if a lung biopsy is taken. This thickened, stiff tissue makes it harder for your lungs to work properly. The most common type of ILD, IPF often gets worse and can't be reversed.
- Cryptogenic organizing pneumonia, also called COP. COP is a rare lung condition in which the small airways, called bronchioles, and tiny air-exchange sacs, called alveoli, get inflamed. This inflammation makes it hard to breathe. Imaging tests show pneumonia, but COP is not an infection, and the cause is not known. Scarring or fibrosis is rare, but it can happen in some patients if the condition comes back.
- Nonspecific interstitial pneumonia. This type of interstitial lung disease causes cells to be inflamed or scar tissue to build up in the spaces between the air sacs in the lungs. It's more likely to happen in people with connective tissue diseases, but it also can be linked to other conditions.
Risk factors
Factors that may make you more likely to get interstitial lung disease include:
- Age. ILD is much more likely to affect adults, although babies and children sometimes get the disease.
- Exposure to toxins at work or in the environment. Working in mining, farming or construction, or for any reason getting exposed to pollutants known to damage lungs, raises your risk of getting ILD.
- Smoking. Some forms of ILD are more likely to occur in people with a history of smoking. Active smoking may make the condition worse, especially if you also have emphysema.
- Radiation and chemotherapy. Having radiation treatments to your chest or using certain chemotherapy drugs raises your risk of lung disease.
- Connective tissue disease. This includes autoimmune diseases that can raise your risk of ILD.
Complications
Interstitial lung disease can lead to a series of life-threatening complications, including:
- High blood pressure in your lungs, also known as pulmonary hypertension. Unlike systemic high blood pressure, this condition affects only the arteries in your lungs. Scar tissue or low oxygen levels restrict the smallest blood vessels, limiting blood flow in your lungs. This raises pressure within the pulmonary arteries and can worsen oxygen exchange, lowering oxygen levels in your blood. Pulmonary hypertension is a serious illness that may get worse over time, causing the right side of your heart to fail.
- Right-sided heart failure, also known as cor pulmonale. This serious condition occurs when your heart's lower right chamber, also known as the right ventricle, must pump harder than usual to move blood through blocked pulmonary arteries. Eventually, the right ventricle fails from the extra strain. This is often due to pulmonary hypertension.
- Respiratory failure. In the end stage of chronic ILD, respiratory failure occurs when severely low blood oxygen levels, along with rising pressures in the pulmonary arteries and the right ventricle, cause the heart to fail.
Prevention
To prevent interstitial lung disease, avoid exposure to toxins at work, such as asbestos, coal dust and silica dust. Also, avoid exposure to toxins in the environment, such as bird protein, mold and bacteria. If you must be around these toxins, protect yourself by wearing a respirator. Other ways to prevent ILD include not smoking and avoiding secondhand smoke.
If you have an autoimmune disease or are taking medicines that raise your risk of getting ILD, talk with your healthcare professional about steps you can take to prevent ILD. Also, get vaccinated because respiratory infections can make symptoms of ILD worse. Be sure you get the pneumonia vaccine and a flu shot each year. Also, ask your healthcare professional about getting vaccinated for pertussis, COVID-19 and respiratory syncytial virus, also called RSV.
Diagnosis

Finding the cause of interstitial lung disease can be challenging, and sometimes the cause can't be found. Many conditions fall into the category of ILD. In addition, the symptoms of a wide range of medical conditions can appear to be ILD. Healthcare professionals must rule out these conditions before making a diagnosis.
Some of the following tests may be necessary.
Lab tests
- Blood tests. Certain bloodwork can detect proteins, antibodies and other markers of autoimmune diseases or inflammatory responses to environmental exposures, such as those caused by molds or bird protein.
Imaging tests
- Computerized tomography, also called a CT scan. This imaging test is key to the diagnosis of interstitial lung disease. It's sometimes the first test in the diagnosis. CT scanners produce 3D images of internal structures. A high-resolution CT scan can be especially helpful in figuring out how much lung damage there is. It can show details of the fibrosis, which can help narrow the diagnosis and guide treatment decisions.
- Echocardiogram. An echocardiogram uses sound waves to visualize the heart. It can create still images of your heart's structures and videos that show how your heart is working. This test can measure the amount of pressure in the right side of your heart.
Pulmonary function tests
- Spirometry and diffusion capacity. This test requires you to breathe out quickly and forcefully through a tube connected to a machine. The machine measures how much air your lungs can hold and how quickly you can move air out of your lungs. It also measures how easily oxygen can move from your lungs into your bloodstream.
- Oximetry. A small device is placed on one of your fingers to measure the oxygen level in your blood. This test may be done at rest or with activity to monitor the course of the lung disease and figure out how serious it is.
Lung tissue analysis
Sometimes interstitial lung diseases can be diagnosed only by looking at a small amount of lung tissue in a lab — what's known as a biopsy.
Your doctor or other healthcare professional may take a tissue sample using one of these methods:
- Bronchoscopy. In this procedure, your healthcare professional removes very small tissue samples — generally no larger than the head of a pin. This is done by using a small, flexible tube, also known as a bronchoscope, that's passed through your mouth or nose into your lungs. The risks of bronchoscopy are generally minor, namely a sore throat for a limited time and hoarseness from the bronchoscope. But the tissue samples are sometimes too small to make a diagnosis.
- Bronchoalveolar lavage. In this procedure, your doctor injects about a tablespoon of sterile salt water through a bronchoscope into a section of your lung and then suctions it out right away. The solution that's removed contains cells from your air sacs. Although bronchoalveolar lavage samples a larger area of the lung than other procedures do, it may not give enough information to find out what's causing pulmonary fibrosis.
- Surgical biopsy. Although this is a more invasive procedure with potential complications, it's often the only way to get a large enough tissue sample to make the correct diagnosis. General anesthesia is used for this test. Surgical instruments and a small camera are inserted through one or more small incisions between the ribs. The camera allows a surgeon to view the lungs on a video monitor while removing tissue samples from the lungs.
Treatment
Lung scarring that already has occurred in interstitial lung disease can't be reversed, and treatment won't always stop the disease from getting worse. Some treatments may make symptoms better for a short time or slow the disease. Others help maintain quality of life.
Because many of the different types of scarring diseases have no approved or proven therapies, clinical trials may be an option to get an experimental treatment.
Medications
Intense research to find treatment options for specific types of interstitial lung disease is ongoing. Treatment may vary depending on the cause of ILD and what damage has happened in the lungs. Using on the latest scientific evidence, your healthcare professional may recommend:
- Corticosteroid medicines. At first, many people diagnosed with ILD are treated with a corticosteroid, namely prednisone (Prednisone Intensol, Rayos). Sometimes people are treated with other drugs that suppress the immune system. Depending on the cause of ILD, these medicines may slow or even keep the disease from getting worse.
- Medicines that slow the worsening of idiopathic pulmonary fibrosis. Pirfenidone (Esbriet) and nintedanib (Ofev) are medicines that may slow the rate at which IPF worsens. Ofev also has been approved for people with lung fibrosis that's getting worse due to other types of interstitial lung disease. Side effects for both drugs are common. Talk with your healthcare professional about the pros and cons of these medicines.
- Medicines that reduce stomach acid. Gastroesophageal reflux disease, also known as GERD, affects most people with idiopathic pulmonary fibrosis. GERD is linked to worse lung damage. If you have symptoms of acid reflux, your healthcare professional may prescribe ways to treat GERD that reduce stomach acid.
Oxygen therapy
Using oxygen can't stop lung damage, but it can:
- Make it easier to breathe and exercise.
- Prevent or lessen complications from low blood oxygen levels.
- Lower blood pressure in the right side of your heart.
- Make your sleep and sense of well-being better.
You're most likely to get oxygen when you sleep or exercise, although some people may use it around the clock.
Pulmonary rehabilitation
The aim of pulmonary rehabilitation is to make you better able to function and live a full, satisfying life. That's why pulmonary rehabilitation programs focus on:
- Learning more about your lung disease.
- Exercise, so you can become more physically active for longer periods of time.
- Breathing techniques that make your lungs more efficient.
- Emotional support.
- Nutritional counseling.
Surgery
A lung transplant may be an option of last resort for some people with severe interstitial lung disease when other treatment options haven't helped.
Lifestyle and home remedies
You must be actively involved in your own treatment and stay as healthy as possible when you're living with interstitial lung disease. For that reason, it's important to:
- Learn about your disease. Understanding your condition and how it can be treated can help you decide about your care. Including family members and friends can help them learn your needs.
- Stop smoking. If you have lung disease, the best thing you can do for yourself is to stop smoking. Talk with your healthcare professional about options for quitting, including programs to help you stop smoking. These programs use various proven techniques to help people quit. And because secondhand smoke also can harm your lungs, don't allow people to smoke around you.
- Avoid exposure at work or during hobbies. When possible, stay away from substances that can irritate your lungs. Ask your healthcare professional for more information and advice.
- Eat well. If you have lung disease, you may lose weight because it isn't comfortable to eat and because of the extra energy it takes to breathe. Aim to eat a nutritionally rich diet that contains enough calories. A dietitian can give you more guidelines for healthy eating.
- Get vaccinated. Respiratory infections can make symptoms of ILD worse. Make sure you get the pneumonia vaccine and a flu shot each year.
Coping and support
Living with a chronic lung disease is emotionally and physically challenging. You may need to change your daily routines and activities — sometimes a lot — as breathing problems worsen or health care needs become more important. Feelings of fear, anger and sadness are typical as you grieve for the loss of your old lifestyle and worry about what's next for you and your family.
Share your feelings with your loved ones and your healthcare professional. Talking openly may help you and your loved ones cope with the emotional challenges of your disease. Also, clear communication can help you and your family plan for your needs if your disease gets worse.
Think about joining a support group, where you can talk with people who are facing challenges like yours. Group members may share coping strategies, exchange information about new treatments or simply listen as you express your feelings. If a group isn't for you, you may want to talk with a counselor in a one-on-one setting.
Preparing for an appointment
You'll probably first see your family healthcare professional about your symptoms. Your family healthcare professional may refer you to a pulmonologist, who is a doctor who specializes in lung diseases.
What you can do
Before your appointment, you might want to prepare answers to these questions:
- What are your symptoms and when did they start?
- Are you being treated for other medical conditions?
- What medicines and supplements have you taken in the past five years, including medicines available without a prescription and street drugs?
- What are all the occupations you've had, even if only for a few months?
- Do any members of your family have a lasting lung disease of any kind?
- Have you ever had chemotherapy or radiation treatments for cancer?
Let your pulmonologist know if you've had any chest X-rays, CT scans or other tests so the healthcare professional can request the results before your visit. The images are more important than the report alone. The pulmonologist can make a diagnosis by comparing an old imaging test with those of a current test.
What to expect from your doctor
Your doctor or other healthcare professional may ask some of these questions:
- Do your symptoms occur all of the time or do they seem to go away and then come back?
- Have you recently had contact with air conditioners, humidifiers, pools, hot tubs, or water-damaged walls or carpet?
- Do you own any pet birds or feather-containing items such as down pillows or comforters?
- Are you exposed to mold or construction dust in your home or other places where you spend a lot of time?
- Have any close relatives, friends or co-workers been diagnosed with a lung condition?
- Do you have any family history of lung disease?
- Does your work history include regularly working with or being around toxins and pollutants, such as asbestos, silica dust or grain dust?
- Do you or did you smoke? If so, how much and for how long? If not, have you spent a lot of time around others who smoke?
- Have you been diagnosed or treated for any other medical conditions, particularly arthritis or rheumatic diseases?
- Do you have symptoms of gastroesophageal reflux disease, also known as GERD, such as heartburn?
© 1998-2026 Mayo Foundation for Medical Education and Research(MFMER). All rights reserved. Terms of Use
