Lupus nephritis
Conditions
Overview
Lupus nephritis is a problem that occurs often in people who have systemic lupus erythematosus, also called lupus.
Lupus is a disease in which the body's immune system attacks its own cells and organs, called autoimmune disease. Lupus causes the immune system to make proteins called autoantibodies. These proteins attack tissues and organs in the body, including the kidneys.
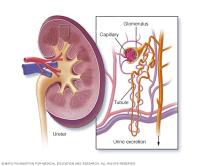
Lupus nephritis occurs when lupus autoantibodies affect parts of the kidneys that filter out waste. This causes swelling and irritation of the kidneys, called inflammation. It might lead to blood in the urine, protein in the urine, high blood pressure, kidneys that don't work well or even kidney failure.
Symptoms
Signs and symptoms of lupus nephritis include:
- Blood in the urine.
- Urine that foams because of too much protein.
- High blood pressure.
- Swelling in the legs, ankles or feet and sometimes in the hands and face.
- High levels of a waste product called creatinine in the blood.
Causes
As many as half of adults with systemic lupus get lupus nephritis. Systemic lupus causes the body's immune system to damage the kidneys. Then the kidneys can't filter out waste as they should.
Risk factors
The only known risk factors for lupus nephritis are:
- Being male. Women are more likely to get lupus, but men get lupus nephritis more than women do.
- Race or ethnicity. Black people, Hispanic people and Asian Americans are more likely to have lupus nephritis than are whites.
Complications
Lupus nephritis can cause:
- Hypertension.
- Kidney failure.
- A higher risk of getting cancer, especially one that starts in the cells of the immune system, called B-cell lymphoma.
- A higher risk of heart and blood vessel problems.
Diagnosis
Tests to diagnose lupus nephritis include:
- Blood and urine tests. Besides the usual blood and urine tests, urine collected over 24 hours might be tested. These tests measure how well the kidneys are working.
- Kidney biopsy. A small section of kidney tissue is removed and sent to a lab. This test diagnoses lupus nephritis. It also can help show how bad the disease is. There can be more than one biopsy over time.
Treatment
There's no cure for lupus nephritis. Treatment aims to:
- Reduce symptoms or make symptoms go away, called remission.
- Keep the disease from getting worse.
- Keep symptoms from coming back.
- Keep kidneys working well enough to not need a machine to filter waste from blood, called dialysis, or a kidney transplant.
Supportive treatments
In general, these treatments might help people with kidney disease:
- Diet changes. Limiting the amount of protein and salt in the diet can help the kidneys work better.
- Blood pressure medicines. Medicines called angiotensin-converting enzyme (ACE) inhibitors and angiotensin II receptor blockers (ARBs) can help control blood pressure. These medicines also keep protein from leaking from the kidneys into the urine. Medicines called diuretics help get rid of fluid.
Medicines
Treating severe lupus nephritis might need medicines that slow or stop the immune system from attacking healthy cells. Medicines often are used together. Sometimes certain medicines used at first are switched to prevent toxic effects.
Medicines to treat lupus nephritis might include:
- Steroids, such as prednisone (Rayos).
- Cyclosporine (Gengraf, Neoral, Sandimmune).
- Voclosporin (Lupkynis).
- Tacrolimus (Astagraf, Envarsus, Prograf).
- Cyclophosphamide (Cytoxan).
- Azathioprine (Azasan, Imuran).
- Mycophenolate (CellCept).
- Rituximab (Rituxan).
- Belimumab (Benlysta).
Ongoing clinical trials are testing new treatments for lupus nephritis.
Treatment options for kidney failure
For people who progress to kidney failure, treatment options include:
- Dialysis. Dialysis helps remove fluid and waste from the body, maintain the right balance of minerals in the blood, and manage blood pressure by filtering the blood through a machine.
- Kidney transplant. If kidneys stop working, a kidney from a donor, called a transplant, might be needed.
© 1998-2026 Mayo Foundation for Medical Education and Research(MFMER). All rights reserved. Terms of Use
