Spinal arteriovenous malformation (AVM)
Conditions
Overview
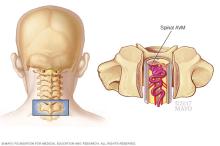
A spinal arteriovenous malformation (AVM) is a tangle of blood vessels that forms on, in or near the spinal cord. This creates irregular connections between arteries and veins. Without treatment, this rare condition can cause lasting damage to the spinal cord.
Oxygen-rich blood enters the spinal cord through arteries. The arteries usually branch into smaller blood vessels called capillaries. The spinal cord gets oxygen from the blood in the capillaries. Then the blood passes into veins and moves away from the spinal cord to the heart and lungs.
But in a spinal AVM, the blood passes directly from the arteries to the veins. This change in blood flow means that the surrounding cells don't get the oxygen they need. This can cause cells in the spinal tissue to weaken or die.
The tangled arteries and veins in a spinal AVM also can burst and cause bleeding in the spinal cord. Sometimes, the AVM gets bigger as blood flow increases. The AVM can press on the spinal cord and cause weakness or other symptoms.
You might not know you have a spinal AVM unless you have symptoms. The condition can be treated with surgery to stop or possibly reverse some of the spinal damage.
Symptoms
Symptoms of a spinal arteriovenous malformation (AVM) can differ from person to person. Symptoms depend on where the AVM is found and how serious it is. Some people may not notice symptoms for many years, if at all. Others may experience symptoms that are life-threatening.
Symptoms often begin when people are in their 20s but can occur at earlier or later ages. Some people are diagnosed under the age of 16.
Symptoms may start suddenly or slowly and may include:
- Trouble walking or climbing stairs.
- Numbness, tingling or sudden pain in the legs.
- Weakness on one or both sides of the body.
As the condition gets worse, you may have more symptoms including:
- Sudden, serious back pain.
- Lack of feeling in the legs.
- Trouble urinating or having bowel movements.
- Headache.
- Stiff neck.
When to see a doctor
Make an appointment with your healthcare professional if you experience symptoms of a spinal AVM.
Causes
The cause of spinal arteriovenous malformations (AVMs) isn't known. Most spinal AVMs are present at birth, known as congenital. But others may happen later in life.
Risk factors
There are no known risk factors for spinal arteriovenous malformations (AVMs). The condition occurs equally in men and women.
Complications
Without treatment, a spinal arteriovenous malformation (AVM) can cause disability that gets worse over time. This is from damage to the spinal cord and surrounding tissues. This can cause:
- Trouble moving.
- Pain, tingling and numbness.
- Damage to the spine.
- Bulging blood vessel, known as an aneurysm.
- High blood pressure in the veins, known as venous hypertension. This can cause fluid to build up, called edema. It also can cause tissues to die due to lack of oxygen, known as spinal cord infarction.
- Hemorrhage, which can speed up spinal cord damage.
Diagnosis
Spinal arteriovenous malformations (AVMs) can be hard to diagnose. The symptoms are similar to those of other spinal conditions. Other conditions may include spinal dural arteriovenous fistula, spinal stenosis, multiple sclerosis or a spinal cord tumor.
Your healthcare professional may recommend tests to help rule out other causes of your symptoms, including:
- Magnetic resonance imaging (MRI), which uses powerful magnets and radio waves to create detailed images of your spinal cord. A spinal MRI can show a mass caused by the irregularly connected blood vessels of an AVM.
-
Angiography, which often is needed to see the location and characteristics of the blood vessels involved in the AVM.
In an angiography, a thin tube called a catheter is inserted into an artery in the groin. It's guided to the spinal cord. Dye is injected into blood vessels in the spinal cord to make them visible under X-ray imaging.
Treatment

Treatment for a spinal arteriovenous malformation (AVM) may involve a combination of approaches. Treatment can lessen symptoms and lower the risk of possible complications. The choice of treatment depends on the size, location and blood flow of the spinal AVM. The results of your neurological exam and your overall health also are taken into account.
The goal of spinal AVM treatment is to lower the risk of the AVM bleeding. Treatment also can stop or prevent disability and other symptoms from getting worse.
Medicines
Pain-relieving medicines may be used to reduce symptoms such as back pain and stiffness. But most spinal AVMs may eventually need surgery.
Surgery
Surgery is often needed to remove a spinal AVM from the surrounding tissue. There are three ways to remove spinal AVMs:
- Conventional surgery. A surgeon makes a cut in the skin to remove the AVM. The surgeon takes care not to damage the spinal cord and surrounding areas. Surgery usually is done when the AVM is fairly small and in an area of the spinal cord that is easy to reach.
-
Endovascular embolization. Endovascular embolization can lower the risk of bleeding and other complications of spinal AVMs.
A catheter is inserted into an artery in the leg. The catheter is then threaded to an artery in the spinal cord that feeds the AVM. Small particles of a gluelike substance are injected. This blocks the artery and reduces blood flow into the AVM. This procedure doesn't permanently destroy the AVM.
You may need endovascular embolization before other types of surgery. This can lower the risk of bleeding during surgery or shrink the AVM so that surgery is more successful.
- Radiosurgery. This procedure uses radiation focused directly on the AVM to destroy the blood vessels of the malformation. Over time, those blood vessels break down and close. Radiosurgery is most often used to treat small AVMs that haven't burst.
Your healthcare team discusses with you the benefits and risks of surgery to remove the spinal AVM. Because the AVM is so close to the spinal cord, spinal AVM surgery is complex. See an experienced neurosurgeon for this type of surgery.
Preparing for an appointment
You may be referred to a doctor who specializes in disorders of the brain and nervous system, known as a neurologist.
What you can do
- Write down your symptoms, including any that may seem unrelated to the reason you scheduled the appointment.
- Make a list of all your medicines, vitamins and supplements.
- Write down your key medical information, including other conditions.
- Write down key personal information, including any recent changes or stressors in your life.
- Write down questions to ask your healthcare professional.
Questions to ask your doctor
- What's the most likely cause of my symptoms?
- What kinds of tests do I need?
- What treatments are available, and what types of side effects can I expect?
- I have other health conditions. How can I best manage these conditions together?
- Should I restrict my activities?
In addition to asking the questions you've prepared, don't hesitate to ask other questions during your appointment.
What to expect from your doctor
You're likely to be asked several questions. Being ready to answer them can allow for more time to go over points you want to discuss in more detail. You may be asked:
- Have you experienced trouble walking or had weakness in your legs?
- Have you had numbness, tingling or pain in your legs?
- Have you had headaches or back pain?
- When did you begin experiencing these symptoms? Have they been continuous or occasional?
- Do your symptoms worsen when you exercise?
© 1998-2026 Mayo Foundation for Medical Education and Research(MFMER). All rights reserved. Terms of Use
