Sclerotherapy
Procedures
Overview
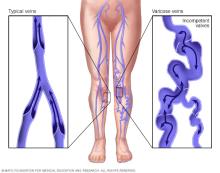
Sclerotherapy treats veins that are twisted and enlarged, known as varicose veins. Varicose veins are usually in the legs. Sclerotherapy also treats spider veins, a mild form of varicose veins. Sclerotherapy usually works best on small varicose veins.
Sclerotherapy involves using a needle to put a solution into the vein. The sclerotherapy solution causes the vein to scar. The scarring forces blood through healthier veins. The varicose vein then fades.
After sclerotherapy, treated veins tend to fade within a few weeks, although they might not go away completely. It can take a month or more for full results. Some varicose veins need more than one sclerotherapy treatment.
Why it's done
Sclerotherapy is usually done to make the veins look better. The procedure also can improve symptoms related to varicose veins, including:
- Aching.
- Swelling.
- Burning.
- Cramping at night.
If you're pregnant or breastfeeding, healthcare professionals suggest waiting to have sclerotherapy done.
Risks
Sclerotherapy generally has few serious complications.
Possible risks of sclerotherapy include:
- Irritation and swelling, called inflammation. You might have mild swelling, warmth and discomfort around the site where the needle went into the skin. Taking a pain reliever you can get without a prescription might help. This includes aspirin or ibuprofen (Advil, Motrin IB, others).
-
Blood clot. If a blood clot forms in a treated vein, it might need to be drained. Rarely, a blood clot can move to a deeper vein in the leg. When this happens, it's called deep vein thrombosis (DVT).
Deep vein thrombosis increases the risk of a blood clot in the lungs, called a pulmonary embolism. It's a very rare complication of sclerotherapy that needs immediate medical care. DVT symptoms include trouble breathing, chest pain or dizziness, or coughing up blood.
- Air bubbles. Tiny air bubbles might collect in the blood. This might not cause symptoms. But symptoms might include flashes in the eyes, headaches, fainting and nausea. These symptoms usually go away. But call your healthcare team if you have trouble moving or if you have a loss of feeling in your arms or legs after the treatment.
- Allergic reaction. An allergic reaction to the solution used for treatment is possible but uncommon.
Also, the needle stick used in sclerotherapy might cause:
- Bruising.
- Hives.
- Small skin sores.
- Darkened skin.
These symptoms usually go away within days to weeks. Some may take longer to go away completely.
How you prepare
To prepare for sclerotherapy, a healthcare professional examines you and asks questions about your medical history. The health professional looks at your veins and checks for blood vessel disease.
Your healthcare team usually asks you about:
- Recent illnesses or medical conditions, such as heart disease or a history of blood clots.
- Allergies.
- Other treatments you've had for varicose veins and the results.
- Medicines or supplements you take, especially aspirin, ibuprofen (Advil, Motrin IB, others), naproxen sodium (Aleve, Anaprox DS), blood thinners, iron supplements or herbal supplements.
Aspirin, ibuprofen, naproxen sodium or blood thinners can increase the risk of bleeding. If you take one or more of these, a member of your healthcare team can tell you how and when to stop taking them before the treatment.
Before sclerotherapy, you might have an ultrasound test of the legs if the veins are causing symptoms.
What you can expect
Sclerotherapy is typically done in a healthcare professional's office. It generally takes an hour or less to do.
Before the procedure
Don't shave your legs or use lotion on them. Wear loose, comfortable clothing.
During the procedure
During sclerotherapy, you lie on your back with your legs slightly raised. A member of your healthcare team cleans the area to be treated. Then your healthcare professional uses a small needle to slowly put solution into the vein.
The solution, usually a liquid, irritates the lining of the vein. It causes the vein to swell shut. This blocks the flow of blood. Eventually the vein disappears.
Some people feel minor stinging or cramping when the needle goes into the vein. Tell your healthcare professional if it hurts a lot. Pain might result from the solution leaking from the vein into the tissue around it.
After the needle is removed, a member of your healthcare team puts pressure on the area and massages it to keep blood out of the vein and to spread the solution. A pad may be taped onto the injection site to keep pressure on the area before moving on to the next vein.
How many times the needle is used to put solution into a vein depends on the number of veins being treated.
After the procedure
You can get up and walk around soon after sclerotherapy. Walking and moving helps keep blood clots from forming.
You usually need to wear compression stockings or bandages for about two weeks. This keeps pressure on the treated veins. Don't shave your leg or use lotion on it until the site heals.
Most people return to their regular activities on the same day. But you might want to have someone drive you home after the treatment. Your healthcare professional might tell you to avoid hard exercise for two weeks after the procedure.
The treated area should stay out of the sun for two weeks. Or use sunscreen with an SPF of at least 30. Being in the sun can lead to dark spots on the treated area, especially for those with Black or brown skin.
Results
Your healthcare team usually asks you to come back for a checkup about a month after your treatment. You usually see the results of sclerotherapy for small varicose veins or spider veins in 3 to 6 weeks. Larger veins might take 3 to 4 months.
Some people need more than one treatment to get the results they want. Generally, you need to wait about six weeks before having another sclerotherapy session.
Varicose veins that go away with treatment generally don't come back. But new ones can appear.
© 1998-2026 Mayo Foundation for Medical Education and Research(MFMER). All rights reserved. Terms of Use
