Arthritis
Conditions
Overview
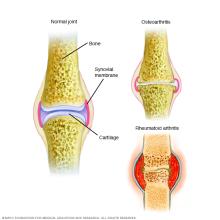
Arthritis is the swelling and tenderness of one or more joints. The main symptoms of arthritis are joint pain and stiffness, which typically worsen with age. The most common types of arthritis are osteoarthritis and rheumatoid arthritis.
Osteoarthritis causes cartilage — the hard, slippery tissue that covers the ends of bones where they form a joint — to break down. Rheumatoid arthritis is a disease in which the immune system attacks the joints, beginning with the lining of joints.
Uric acid crystals, which form when there's too much uric acid in your blood, can cause gout. Infections or underlying disease, such as psoriasis or lupus, can cause other types of arthritis.
Treatments vary depending on the type of arthritis. The main goals of arthritis treatments are to reduce symptoms and improve quality of life.
Symptoms
The most common signs and symptoms of arthritis involve the joints. Depending on the type of arthritis, signs and symptoms may include:
- Pain
- Stiffness
- Swelling
- Redness
- Decreased range of motion
Causes
The two main types of arthritis — osteoarthritis and rheumatoid arthritis — damage joints in different ways.
Osteoarthritis
The most common type of arthritis, osteoarthritis involves wear-and-tear damage to a joint's cartilage — the hard, slick coating on the ends of bones where they form a joint. Cartilage cushions the ends of the bones and allows nearly frictionless joint motion, but enough damage can result in bone grinding directly on bone, which causes pain and restricted movement. This wear and tear can occur over many years, or it can be hastened by a joint injury or infection.
Osteoarthritis also causes changes in the bones and deterioration of the connective tissues that attach muscle to bone and hold the joint together. If cartilage in a joint is severely damaged, the joint lining may become inflamed and swollen.
Rheumatoid arthritis
In rheumatoid arthritis, the body's immune system attacks the lining of the joint capsule, a tough membrane that encloses all the joint parts. This lining (synovial membrane) becomes inflamed and swollen. The disease process can eventually destroy cartilage and bone within the joint.
Risk factors
Risk factors for arthritis include:
- Family history. Some types of arthritis run in families, so you may be more likely to develop arthritis if your parents or siblings have the disorder.
- Age. The risk of many types of arthritis — including osteoarthritis, rheumatoid arthritis and gout — increases with age.
- Your sex. Women are more likely than men to develop rheumatoid arthritis, while most of the people who have gout, another type of arthritis, are men.
- Previous joint injury. People who have injured a joint, perhaps while playing a sport, are more likely to eventually develop arthritis in that joint.
- Obesity. Carrying excess pounds puts stress on joints, particularly your knees, hips and spine. People with obesity have a higher risk of developing arthritis.
Complications
Severe arthritis, particularly if it affects your hands or arms, can make it difficult for you to do daily tasks. Arthritis of weight-bearing joints can keep you from walking comfortably or sitting up straight. In some cases, joints may gradually lose their alignment and shape.
Diagnosis
During the physical exam, doctors check your joints for swelling, redness and warmth. They'll also want to see how well you can move your joints.
Laboratory tests
The analysis of different types of body fluids can help pinpoint the type of arthritis you may have. Fluids commonly analyzed include blood, urine and joint fluid. To obtain a sample of joint fluid, doctors cleanse and numb the area before inserting a needle in the joint space to withdraw some fluid.
Imaging
These types of tests can detect problems within the joint that may be causing your symptoms. Examples include:
- X-rays. Using low levels of radiation to visualize bone, X-rays can show cartilage loss, bone damage and bone spurs. X-rays may not reveal early arthritic damage, but they are often used to track progression of the disease.
- Computerized tomography (CT). CT scanners take X-rays from many different angles and combine the information to create cross-sectional views of internal structures. CTs can visualize both bone and the surrounding soft tissues.
- Magnetic resonance imaging (MRI). Combining radio waves with a strong magnetic field, MRIs can produce more-detailed cross-sectional images of soft tissues such as cartilage, tendons and ligaments.
- Ultrasound. This technology uses high-frequency sound waves to image soft tissues, cartilage and fluid-containing structures near the joints (bursae). Ultrasound is also used to guide needle placement for removing joint fluid or injecting medications into the joint.
Treatment
Arthritis treatment focuses on relieving symptoms and improving joint function. You may need to try several different treatments, or combinations of treatments, before you determine what works best for you.
Medications
The medications used to treat arthritis vary depending on the type of arthritis. Commonly used arthritis medications include:
- NSAIDs. Nonsteroidal anti-inflammatory drugs (NSAIDs) can relieve pain and reduce inflammation. Examples include ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve). Stronger NSAIDs can cause stomach irritation and may increase your risk of heart attack or stroke. NSAIDs are also available as creams or gels, which can be rubbed on joints.
- Counterirritants. Some varieties of creams and ointments contain menthol or capsaicin, the ingredient that makes hot peppers spicy. Rubbing these preparations on the skin over your aching joint may interfere with the transmission of pain signals from the joint itself.
- Steroids. Corticosteroid medications, such as prednisone, reduce inflammation and pain and slow joint damage. Corticosteroids may be given as a pill or as an injection into the painful joint. Side effects may include thinning of bones, weight gain and diabetes.
- Disease-modifying antirheumatic drugs (DMARDs). These drugs can slow the progression of rheumatoid arthritis and save the joints and other tissues from permanent damage. In addition to conventional DMARDs, there are also biologic agents and targeted synthetic DMARDs. Side effects vary but most DMARDs increase your risk of infections.
Therapy
Physical therapy can be helpful for some types of arthritis. Exercises can improve range of motion and strengthen the muscles surrounding joints. In some cases, splints or braces may be warranted.
Surgery
If conservative measures don't help, doctors may suggest surgery, such as:
- Joint repair. In some instances, joint surfaces can be smoothed or realigned to reduce pain and improve function. These types of procedures can often be performed arthroscopically — through small incisions over the joint.
- Joint replacement. This procedure removes the damaged joint and replaces it with an artificial one. Joints most commonly replaced are hips and knees.
- Joint fusion. This procedure is more often used for smaller joints, such as those in the wrist, ankle and fingers. It removes the ends of the two bones in the joint and then locks those ends together until they heal into one rigid unit.
Lifestyle and home remedies
In many cases, arthritis symptoms can be reduced with the following measures:
- Weight loss. Excess weight puts extra stress on weight-bearing joints. Losing weight may increase your mobility and limit future joint injury.
- Exercise. Regular exercise can help keep joints flexible. Swimming and water aerobics may be good choices because the buoyancy of the water reduces stress on weight-bearing joints.
- Heat and cold. Heating pads or ice packs may help relieve arthritis pain.
- Assistive devices. Using canes, shoe inserts, walkers, raised toilet seats, and other assistive devices can help protect joints and improve your ability to perform daily tasks.
Alternative medicine
Many people use alternative remedies for arthritis, but there is little reliable evidence to support the use of many of these products. The most promising alternative remedies for arthritis include:
- Acupuncture. This therapy uses fine needles inserted at specific points on the skin to reduce many types of pain, including that caused by some types of arthritis.
- Glucosamine. Although study results have been mixed, some studies have found that glucosamine works no better than placebo. However, glucosamine and the placebo both relieved osteoarthritis pain better than taking nothing, particularly in people who have moderate to severe pain from knee osteoarthritis.
- Chondroitin. Chondroitin may provide modest pain relief from osteoarthritis, although study results are mixed.
- Fish oil. Some preliminary studies have found that fish oil supplements may reduce the symptoms of some types of arthritis. Fish oil can interfere with medications, so check with your doctor first.
- Yoga and tai chi. The slow, stretching movements associated with yoga and tai chi may help improve joint flexibility and range of motion.
- Massage. Light stroking and kneading of muscles may increase blood flow and warm affected joints, temporarily relieving pain. Make sure your massage therapist knows which joints are affected by arthritis.
Preparing for an appointment
While you might first discuss your symptoms with your family doctor, he or she may refer you to a doctor who specializes in the treatment of joint problems (rheumatologist) for further evaluation.
What you can do
Before your appointment, make a list that includes:
- Detailed descriptions of your symptoms
- Information about medical problems you've had in the past
- Information about the medical problems of your parents or siblings
- All the medications and dietary supplements you take
- Questions you want to ask the doctor
What to expect from your doctor
Your doctor may ask some of the following questions:
- When did your symptoms start?
- Does activity make the pain better or worse?
- Which joints are painful?
- Do you have a family history of joint pain?
© 1998-2026 Mayo Foundation for Medical Education and Research(MFMER). All rights reserved. Terms of Use
