Colonoscopy
Procedures
Overview
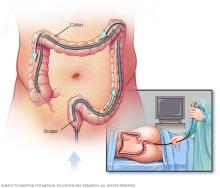
A colonoscopy (koe-lun-OS-kuh-pee) is an exam used to look for changes — such as swollen, irritated tissues, polyps or cancer — in the large intestine (colon) and rectum.
During a colonoscopy, a long, flexible tube (colonoscope) is inserted into the rectum. A tiny video camera at the tip of the tube allows the doctor to view the inside of the entire colon.
If necessary, polyps or other types of abnormal tissue can be removed through the scope during a colonoscopy. Tissue samples (biopsies) can be taken during a colonoscopy as well.
Why it's done
Your doctor may recommend a colonoscopy to:
- Investigate intestinal signs and symptoms. A colonoscopy can help your doctor explore possible causes of abdominal pain, rectal bleeding, chronic diarrhea and other intestinal problems.
- Screen for colon cancer. If you're age 45 or older and at average risk of colon cancer — you have no colon cancer risk factors other than age — your doctor may recommend a colonoscopy every 10 years. If you have other risk factors, your doctor may recommend a screen sooner. Colonoscopy is one of a few options for colon cancer screening. Talk with your doctor about the best options for you.
- Look for more polyps. If you have had polyps before, your doctor may recommend a follow-up colonoscopy to look for and remove any additional polyps. This is done to reduce your risk of colon cancer.
- Treat an issue. Sometimes, a colonoscopy may be done for treatment purposes, such as placing a stent or removing an object in your colon.
Risks
A colonoscopy poses few risks. Rarely, complications of a colonoscopy may include:
- A reaction to the sedative used during the exam
- Bleeding from the site where a tissue sample (biopsy) was taken or a polyp or other abnormal tissue was removed
- A tear in the colon or rectum wall (perforation)
After discussing the risks of colonoscopy with you, your doctor will ask you to sign a consent form giving permission for the procedure.
How you prepare
Before a colonoscopy, you'll need to clean out (empty) your colon. Any residue in your colon may make it difficult to get a good view of your colon and rectum during the exam.
To empty your colon, your doctor may ask you to:
- Follow a special diet the day before the exam. Typically, you won't be able to eat solid food the day before the exam. Drinks may be limited to clear liquids — plain water, tea and coffee without milk or cream, broth, and carbonated beverages. Avoid red liquids, which can be mistaken for blood during the colonoscopy. You may not be able to eat or drink anything after midnight the night before the exam.
- Take a laxative. Your doctor will usually recommend taking a prescription laxative, usually in a large volume in either pill form or liquid form. In most instances, you will be instructed to take the laxative the night before your colonoscopy, or you may be asked to use the laxative both the night before and the morning of the procedure.
-
Adjust your medications. Remind your doctor of your medications at least a week before the exam — especially if you have diabetes, high blood pressure or heart problems or if you take medications or supplements that contain iron.
Also tell your doctor if you take aspirin or other medications that thin the blood, such as warfarin (Coumadin, Jantoven); newer anticoagulants, such as dabigatran (Pradaxa) or rivaroxaban (Xarelto), used to reduce risk of blot clots or stroke; or heart medications that affect platelets, such as clopidogrel (Plavix).
You may need to adjust your dosages or stop taking the medications temporarily.
What you can expect
During the procedure
During a colonoscopy, you'll wear a gown, but likely nothing else. Sedation or anesthesia is usually recommended. In most cases, the sedative is combined with pain medication given directly into your blood stream (intravenously) to lessen any discomfort.
You'll begin the exam lying on your side on the exam table, usually with your knees drawn toward your chest. The doctor will insert a colonoscope into your rectum.
The scope — which is long enough to reach the entire length of your colon — contains a light and a tube (channel) that allows the doctor to pump air, carbon dioxide or water into your colon. The air or carbon dioxide inflates the colon, which provides a better view of the lining of the colon.
When the scope is moved or air is introduced, you may feel stomach cramping or the urge to have a bowel movement.
The colonoscope also contains a tiny video camera at its tip. The camera sends images to an external monitor so that the doctor can study the inside of your colon.
The doctor can also insert instruments through the channel to take tissue samples (biopsies) or remove polyps or other areas of abnormal tissue.
A colonoscopy typically takes about 30 to 60 minutes.
After the procedure
After the exam, it takes about an hour to begin to recover from the sedative. You'll need someone to take you home because it can take up to a day for the full effects of the sedative to wear off. Don't drive or make important decisions or go back to work for the rest of the day.
You may feel bloated or pass gas for a few hours after the exam, as you clear the air from your colon. Walking may help relieve any discomfort.
You may also notice a small amount of blood with your first bowel movement after the exam. Usually this isn't cause for alarm. Consult your doctor if you continue to pass blood or blood clots or if you have persistent abdominal pain or a fever. While unlikely, this may occur immediately or in the first few days after the procedure, but may be delayed for up to 1 to 2 weeks.
Results
Your doctor will review the results of the colonoscopy and then share the results with you.
Negative result
A colonoscopy is considered negative if the doctor doesn't find any abnormalities in the colon.
Your doctor may recommend that you have another colonoscopy:
- In 10 years, if you're at average risk of colon cancer and you have no colon cancer risk factors other than age or if you have benign small polyps.
- In 1 to 7 years, depending on a variety of factors: The number, size and type of polyps removed; if you have a history of polyps in previous colonoscopy procedures; if you have certain genetic syndromes; or if you have a family history of colon cancer.
If there was residual stool in the colon that prevented complete examination of your colon, your doctor may recommend a repeat colonoscopy. How soon will depend on the amount of stool and how much of your colon was able to be seen. Your doctor may recommend a different bowel preparation to ensure that your bowel is completely emptied before the next colonoscopy.
Positive result
A colonoscopy is considered positive if the doctor finds any polyps or abnormal tissue in the colon.
Most polyps aren't cancerous, but some can be precancerous. Polyps removed during colonoscopy are sent to a laboratory for analysis to determine whether they are cancerous, precancerous or noncancerous.
Depending on the size and number of polyps, you may need to follow a more rigorous surveillance schedule in the future to look for more polyps.
If your doctor finds one or two polyps less than 0.4 inch (1 centimeter) in diameter, he or she may recommend a repeat colonoscopy in 7 to 10 years, depending on your other risk factors for colon cancer.
Your doctor will recommend another colonoscopy sooner if you have:
- More than two polyps
- A large polyp — larger than 0.4 inch (1 centimeter)
- Polyps and also residual stool in the colon that prevents complete examination of the colon
- Polyps with certain cell characteristics that indicate a higher risk of future cancer
- Cancerous polyps
If you have a polyp or other abnormal tissue that couldn't be removed during the colonoscopy, your doctor may recommend a repeat exam with a gastroenterologist who has special expertise in removing large polyps, or surgery.
Problems with your exam
If your doctor is concerned about the quality of the view through the scope, he or she may recommend a repeat colonoscopy or a shorter time until your next colonoscopy. If your doctor was unable to advance the scope through your entire colon, a virtual colonoscopy may be recommended to examine the rest of your colon.
© 1998-2026 Mayo Foundation for Medical Education and Research(MFMER). All rights reserved. Terms of Use
