Benign paroxysmal positional vertigo (BPPV)
Conditions
Overview
Benign paroxysmal positional vertigo, also called BPPV, is one of the most common causes of vertigo. Vertigo is the sudden feeling of spinning or moving.
BPPV causes brief periods of mild to intense dizziness. Certain changes in the head's position most often set them off. This might happen from tipping the head up or down, lying down, or turning over or sitting up in bed.
Although BPPV can be a bother, it's rarely serious. But it can raise the chance of falling. A healthcare professional can treat BPPV during an office visit.
Symptoms
The symptoms of benign paroxysmal positional vertigo, also called BPPV, may include:
- Dizziness.
- A sense of spinning or moving or that the area around you is spinning or moving. This is called vertigo.
- A loss of balance or not being steady.
- Stomach upset and vomiting.
The symptoms of BPPV can come and go. Symptoms most often last less than a minute. Bouts of BPPV can go away for some time and then come back.
What type of head movement brings on BPPV varies from person to person. But a change in head position almost always is what brings on the symptoms. Some people also feel off balance when standing or walking.
Atypical rhythmic eye movements, called nystagmus, most often go with the symptoms of benign paroxysmal positional vertigo.
When to see a doctor
See your healthcare professional if you have dizziness or vertigo that is sudden, intense, lasts long or keeps coming back.
Seek emergency care
It's not common for BPPV to signal a serious illness. But see your healthcare professional right away if you have dizziness or vertigo with any of the following:
- A new, different or bad headache.
- A fever.
- Seeing double or not being able to see well.
- Hearing loss.
- Trouble talking.
- Weakness in the leg or arm.
- Passing out.
- Falling or trouble walking.
- Numbness or tingling.
Causes
Often, there's no known cause for BPPV. This is called idiopathic BPPV.
When there is a known cause, BPPV may be linked with a blow to the head. Less common causes of BPPV include conditions that damage the inner ear.
Rarely, the cause can be damage that happens during ear surgery. Or the symptoms can result from being on your back for a time, such as during surgery or bed rest.
The ear's role
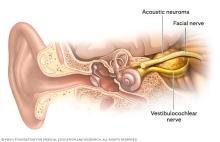
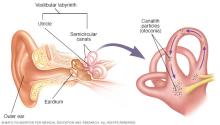
Inside the ear is a tiny organ called the vestibular labyrinth. It includes three loop-shaped structures called semicircular canals. They have fluid and fine, hairlike sensors that detect the head's movement.
Other structures in the ear, called otolith organs, detect the head's movements up and down, right and left, back and forth. The otolith organs hold crystals that respond to gravity.
For many reasons, these crystals can move out of place. When the crystals move, they can go into one of the semicircular canals. Certain head movements can cause the crystals to move.
When the crystals move, they cause the semicircular canal to become sensitive to certain head position changes. This is what causes the dizziness.
Risk factors
The risk of benign paroxysmal positional vertigo is higher in people age 50 and older. But it can happen at any age. The condition is more common in people assigned female at birth.
A head injury or any other condition of the balance organs of the ear may raise the risk of BPPV. The bone-thinning condition osteoporosis also might be a risk factor.
Complications
BPPV rarely causes complications. The dizziness of BPPV can make you unsteady, which may raise your risk of falling and injury from falls.
Diagnosis
To diagnose benign paroxysmal positional vertigo, also called BPPV, your healthcare professional does a physical exam and moves your head into different positions and looks for:
- Symptoms of dizziness that start from eye or head movements and then ease in less than one minute.
- Dizziness with certain head movements. These happen when you lie on your back with your head turned to one side and tipped slightly over the edge of the exam table.
- Eye movements that happen on their own, called nystagmus.
If your healthcare professional can't find the cause of your symptoms, you may need more tests, such as:
- Electronystagmography, also called ENG, or videonystagmography, also called VNG. These tests show atypical eye movement, called nystagmus. ENG uses electrodes. VNG uses small cameras. Either test can help show if an inner ear condition is causing your dizziness.
- MRI. This test uses a magnetic field and radio waves to make images of your head and body. These images can help diagnose a range of conditions. You might have an MRI to rule out other causes of vertigo.
Treatment
Benign paroxysmal positional vertigo may go away on its own within a few weeks or months. To help relieve BPPV, your healthcare professional, audiologist or physical therapist may treat you with a series of movements called the canalith repositioning procedure.
Canalith repositioning
Done in your healthcare professional's office, the canalith repositioning procedure involves simple, slow head movements. There are several types of repositioning procedures that a healthcare professional may do. The goal is to move crystals from the fluid-filled semicircular canals of the inner ear into a part of the ear where they won't cause dizziness.
You hold each position for about 30 seconds after symptoms or atypical eye movements stop. This procedure most often works after one or two treatments.
Your healthcare professional can teach you how to do the procedure on yourself. Then you can do it at home if needed.
Surgery
Rarely, when the canalith repositioning procedure doesn't work, your healthcare professional may suggest a surgical procedure. The surgery may involve putting in a bone plug to block the part of the inner ear that's causing dizziness. The plug keeps the semicircular canal in the ear from responding to particle movements or all head movements.
Lifestyle and home remedies
If you have dizziness because of BPPV, work with your healthcare professional to manage your symptoms. And think about the following:
- Be aware that you might lose your balance. This can cause you to fall, which can cause serious injury.
- Don't move in ways that bring on the symptoms.
- Sit down right away when you feel dizzy.
- Use good lighting if you get up at night.
- Walk with a cane if you're at risk of falling.
Preparing for an appointment
Make an appointment with your main healthcare professional if you have symptoms of BPPV. Your healthcare professional may send you to an ear, nose and throat specialist, also called an ENT, or a doctor who specializes in the brain and nervous system, called a neurologist.
Here's some information to help you get ready for your appointment.
What you can do
- Write down your symptoms, including when they started and how often you have them.
- Note any recent blows to your head, including even minor injuries.
- Make a list of your key medical information. Including any other conditions for which you're being treated and the names and dosages of any medicines, vitamins or supplements you take.
- Write down questions to ask your healthcare professional. Writing down your questions can help you make the most of your appointment time.
Questions to ask at the first appointment include:
- What are the possible causes of my symptoms?
- What tests do you suggest?
- If these tests don't find the cause of my symptoms, what other tests might I need?
- Do I need to follow any restrictions while waiting for a diagnosis?
- Should I see a specialist?
Questions to ask if you are referred to a specialist include:
- What treatments are most likely to help me feel better?
- How soon after I start treatment might my symptoms start to improve?
- If the first treatment doesn't work, what would you suggest next?
- What self-care steps can help me manage this condition?
- Do I need to restrict my activities? For how long?
- Am I at risk of this condition coming back?
- What handouts or websites do you suggest for learning more about BPPV?
What to expect from your doctor
Your healthcare professional might ask you questions, such as:
- Do your symptoms come and go? How often?
- How long do your symptoms last?
- What seems to set off your symptoms, such as certain types of movement or activity?
- Do your symptoms include vision issues?
- Do your symptoms include nausea or vomiting?
- Do your symptoms include headache?
- Have you lost any hearing?
© 1998-2026 Mayo Foundation for Medical Education and Research(MFMER). All rights reserved. Terms of Use
