Chronic traumatic encephalopathy
Conditions
Overview
Chronic traumatic encephalopathy, also known as CTE, is a brain disease likely caused by repeated head injuries. It causes the death of nerve cells in the brain, known as degeneration. CTE gets worse over time. The only way to definitively diagnosis CTE is after death during an autopsy of the brain.
CTE is rare and not well understood, but experts don't believe it's related to a single head injury. CTE appears to be related to repeated head injuries, often occurring in contact sports or military combat. CTE also has been associated with second impact syndrome, when a second head injury occurs before symptoms of a previous head injury have fully resolved.
Experts are still trying to understand how repeated head injuries and other factors might contribute to the changes in the brain that result in CTE. Researchers are looking at how the number of head injuries someone experiences and how bad the injuries are may affect risk of CTE. Experts also don't yet know how often CTE occurs in the population.
CTE has been found in the brains of people who played U.S. football and other contact sports, including boxing. It also may occur in military members who were exposed to explosive blasts. Symptoms of CTE are thought to include trouble with thinking and emotions, physical symptoms, and other behaviors. It's thought that symptoms develop years to decades after head trauma occurs.
Researchers are working on developing tests for CTE, but none has been validated yet. Healthcare professionals may diagnose traumatic encephalopathy syndrome when the symptoms associated with CTE occur together. There is no cure for CTE.
Symptoms
There are no specific symptoms that have been clearly linked to chronic traumatic encephalopathy, also known as CTE. Some of the possible symptoms can occur in many other conditions. In people who were confirmed to have CTE at autopsy, symptoms have included cognitive, behavioral, mood and movement changes.
Cognitive impairment
- Trouble thinking.
- Memory loss.
- Problems with planning, organizing and carrying out tasks.
Behavioral changes
- Impulsive behavior.
- Aggression.
Mood changes
- Depression or apathy.
- Emotional instability.
- Substance misuse.
- Suicidal thoughts or behavior.
Movement symptoms
- Trouble with walking and with balance.
- Shaking, slow movement and trouble with speech, known as parkinsonism.
- Gradual loss of control of movements, such as walking, speaking, swallowing and breathing, known as motor neuron disease.
CTE symptoms don't develop right after a head injury. Experts believe that they develop over years or decades after repeated head trauma.
Experts also believe that CTE symptoms appear in two forms. In early life between the late 20s and early 30s, the first form of CTE may cause mental health and behavioral issues. Symptoms of this form include depression, anxiety, impulsive behavior and aggression. The second form of CTE is thought to cause symptoms later in life, around age 60. These symptoms include trouble with memory and thinking that is likely to progress to dementia.
The full list of signs to look for in people with CTE at autopsy is still unknown. There's also little known about how CTE progresses.
When to see a doctor
CTE is thought to develop over many years after repeated brain injuries that may be mild or severe. See your healthcare professional in these situations:
- Suicidal thoughts. Research shows that people with CTE may be at increased risk of suicide. If you have thoughts of hurting yourself, call 911 or your local emergency number. Or contact a suicide hotline. In the U.S., call or text 988 to reach the 988 Suicide & Crisis Lifeline or use the Lifeline Chat.
- Head injury. See your healthcare professional if you've had a head injury, even if you didn't need emergency care. If your child has had a head injury that concerns you, call your child's healthcare professional right away. Depending on the symptoms, your child's health professional may recommend seeking immediate medical care.
- Memory problems. See your healthcare professional if you have memory loss or if you have other thinking or behavior symptoms.
- Personality or mood changes. Also see your healthcare professional if you feel depressed, anxious, aggressive or impulsive.
Causes
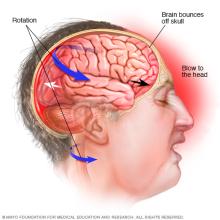
Repeated head trauma is likely the cause of chronic traumatic encephalopathy, also known as CTE. Football players in the United States, ice hockey players and military members serving in war zones have been the focus of most CTE studies. However, other sports and factors such as physical abuse can lead to repeated head injuries. Research also has found that CTE can affect people who played both amateur and professional sports. This was discovered when autopsies were done of the brains of young people who had died and had repeated head injuries during their lives.
A head injury can cause a concussion, which may lead to headaches, trouble with memory and other symptoms. Not everyone who experiences repeated concussions, including athletes and military members, goes on to develop CTE. Some studies have shown no increased incidence of CTE in people exposed to repeated head injuries.
In brains with CTE, researchers have found that there is a buildup of a protein called tau around the blood vessels. Tau buildup in CTE is different from tau buildup in Alzheimer's disease and other forms of dementia. CTE is thought to cause areas of the brain to waste away, known as atrophy. This happens because injuries to nerve cells that conduct electrical impulses affect communication between cells.
It's possible that people with CTE may show signs of another neurodegenerative disease, such as Alzheimer's disease, amyotrophic lateral sclerosis (ALS), Parkinson's disease or frontotemporal dementia.
Risk factors
Repeated traumatic brain injuries are thought to increase the risk of chronic traumatic encephalopathy. Experts are still learning about the risk factors.
Prevention
Chronic traumatic encephalopathy, also known as CTE, can be prevented by lowering the risk of getting a concussion. People who have had one concussion are more likely to have another head injury. The current recommendation to prevent CTE is to reduce mild traumatic brain injuries and to prevent additional injury after a concussion.
Diagnosis
There is no way to definitively diagnose chronic traumatic encephalopathy, also known as CTE, during life. But experts have developed clinical criteria for traumatic encephalopathy syndrome, also known as TES. The syndrome is a group of symptoms that occur together and are associated with CTE.
Healthcare professionals may suspect you have CTE if you meet criteria for TES and have had repeated head trauma over years during sports or military experiences. A diagnosis requires evidence of degeneration of brain tissue and deposits of tau and other proteins in the brain. This can only be seen after death during an autopsy.
Some researchers are actively trying to find a test for CTE that can be used while people are alive. Others continue to study the brains of deceased individuals who may have had CTE, such as U.S. football players.
The hope is to eventually use neuropsychological tests, brain imaging such as specialized MRI and other biomarkers to diagnose CTE.
Treatment
There is no treatment for chronic traumatic encephalopathy, and symptoms continue to get worse over time. More research on treatments is needed, but the current approach is to prevent head injury.
It's also important to stay informed about how to detect and manage traumatic brain injury. Therapies such as cognitive behavioral therapy and medicines may help symptoms of depression and anxiety.
Preparing for an appointment
You'll probably start by seeing your healthcare professional. You then may be referred to a specialist trained in nervous system conditions, known as a neurologist, or a doctor who specializes in mental health, known as a psychiatrist, for an evaluation. Or you may be referred to a specialist in neurology and psychology, known as a neuropsychologist, or other specialists for further evaluation.
What you can do
You can do the following to get ready for your appointment:
- Be aware of any pre-appointment restrictions. At the time you make the appointment, be sure to ask if there's anything you need to do in advance. For example, ask if you need to fast for blood tests.
- Write down any symptoms, including any that may not seem related to the reason you scheduled the appointment. Your healthcare professional will likely want to know details about your mental function. Try to remember when you first started to suspect that something might be wrong. If you think your symptoms are getting worse, write down why and include specific examples.
- Write down key personal information, including any major stresses or recent life changes.
- Make a list of all medicines, vitamins or supplements that you're taking.
- Make a list of your other medical conditions. Include conditions you are currently being treated for, such as if you have diabetes or heart disease. And list any conditions you've had in the past, such as strokes.
- Take a family member, friend or caregiver along, if possible. Sometimes it can be hard to recall all the information provided during an appointment. Someone who comes with you may remember something that you missed or forgot.
Prepare a list of questions before your appointment. List your questions from most important to least important. This can help make the most of your time with the healthcare professional. Some basic questions to ask your healthcare professional include:
- What is likely causing my symptoms? Are there other possible causes for my symptoms?
- What kinds of tests do I need?
- Is my condition likely temporary or long-lasting? How might it progress over time?
- What's the best course of action?
- What are the alternatives to the primary approach being suggested?
- I have other medical issues. How can they be managed together?
- Are there any restrictions?
Other basic questions to ask include:
- If medicine is being prescribed, is there a potential interaction with other medicines I am taking?
- Are there any clinical trials of experimental treatments I should consider?
- Are there any brochures or other printed material that I can take home with me? What websites do you recommend?
- Do I need to see a specialist? What will that cost, and will my insurance cover it? You may need to call your insurance provider for answers to some of these questions.
If you've had a concussion, some basic questions to ask your doctor include:
- What is the risk of future concussions?
- When will it be safe to return to competitive sports?
- When will it be safe to resume vigorous exercise?
- Is it safe to return to school or work?
- Is it safe to drive a car or operate power equipment?
Don't hesitate to ask questions during your appointment at any time that you don't understand something.
What to expect from your doctor
Your healthcare professional may ask you a variety of questions.
Questions related to symptoms:
- What symptoms are you having? Any trouble with word use, memory, focus, personality or directions?
- When did symptoms begin?
- Are symptoms steadily worsening, or are they sometimes better and sometimes worse?
- How severe are your symptoms?
- Have you stopped doing certain activities, such as managing finances or shopping, because of trouble thinking through them?
- What, if anything, seems to improve or worsen symptoms?
Other questions you may be asked related to symptoms:
- Have you noticed any changes in the way you tend to react to people or events?
- Do you have more energy than usual, less than usual or about the same?
- Have you noticed any trembling or trouble walking?
Questions related to health history:
- Have you had your hearing and vision tested recently?
- Is there a family history of dementia or other neurological disease such as Alzheimer's disease, ALS or Parkinson's disease?
- What medicines are you taking? Are you taking any vitamins or supplements?
- Do you drink alcohol? How much?
- What other medical conditions are you being treated for?
If you've had a concussion, your healthcare professional may ask questions related to events surrounding the injury:
- Have you had any previous head injuries?
- Do you play contact sports?
- How did you get this injury?
- What symptoms did you have immediately after the injury?
- Do you remember what happened right before and after the injury?
- Did you lose consciousness after the injury?
- Did you have seizures?
Questions related to physical symptoms:
- Have you experienced nausea or vomiting since the injury?
- Have you been experiencing headaches? How soon after the injury did the headaches start?
- Have you noticed any changes with your physical coordination since the injury?
- Have you noticed any sensitivity or problems with your vision and hearing?
- Have you noticed changes in your sense of smell or taste?
- How is your appetite?
More questions related to physical symptoms:
- Have you been easily fatigued since the injury?
- Are you having trouble sleeping or waking from sleep?
- Do you have any dizziness or vertigo?
Questions related to cognitive or emotional symptoms:
- Have you had any symptoms related to memory or concentration since the injury?
- Have you had any mood changes, including irritability, anxiety or depression?
- Have you had any thoughts about hurting yourself or others?
- Have you noticed or have others commented that your personality has changed?
- What other symptoms are you concerned about?
© 1998-2026 Mayo Foundation for Medical Education and Research(MFMER). All rights reserved. Terms of Use
