Coarctation of the aorta
Conditions
Overview
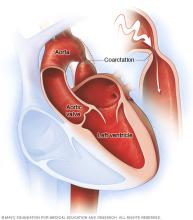
Aortic coarctation (ko-ahrk-TAY-shun) is a narrowing of a part of the body's main artery, called the aorta. The condition forces the heart to work harder to pump blood.
Coarctation of the aorta is usually present at birth. That means it is a congenital heart defect. But sometimes the condition can occur later in life.
Coarctation of the aorta often occurs along with other congenital heart defects. Treatment to fix the condition is usually successful. But regular health checkups are needed for life to watch for changes in the heart's health.
Symptoms
Symptoms of coarctation of the aorta depend on how much of the aorta is narrowed. Most people don't have symptoms.
Adults and older children with mild coarctation of the aorta may not have symptoms and their hearts may seem healthy.
If a baby is born with an extreme narrowing of the aorta, symptoms may be noticed shortly after birth. Symptoms of coarctation of the aorta in infants include:
- Difficulty breathing.
- Difficulty feeding.
- Heavy sweating.
- Irritability.
- Changes in skin color.
Symptoms of coarctation of the aorta later in life may include:
- Chest pain.
- High blood pressure.
- Headaches.
- Muscle weakness.
- Leg cramps.
- Cold feet.
- Nosebleeds.
Coarctation of the aorta often occurs with other heart conditions present at birth. Other symptoms depend on the specific types of congenital heart defects.
When to see a doctor
Get medical help right away for any chest pain that is extreme or can't be explained.
Also get medical help for these symptoms:
- Fainting.
- Sudden shortness of breath.
- High blood pressure that can't be explained.
These symptoms can be caused by many different health conditions. A complete health checkup is needed to learn the cause.
Causes
The cause of coarctation of the aorta is unclear. It's usually a heart problem present at birth, called a congenital heart defect. A congenital heart defect happens as the baby is growing in the womb during pregnancy. The cause is often unknown.
Rarely, coarctation of the aorta can happen later in life. Conditions or events that can narrow the aorta and cause this condition include:
- Traumatic injury.
- An extreme buildup of cholesterols and fats in the arteries, called atherosclerosis.
- A rare type of swelling and irritation of blood vessels in the heart, called Takayasu arteritis.
Risk factors
Risk factors for coarctation of the aorta include:
- Male sex.
- Some genetic conditions, such as Turner syndrome.
- Some heart conditions present at birth, called congenital heart defects.
Congenital heart defects associated with coarctation of the aorta include:
- Bicuspid aortic valve. The aortic valve is between the body's main artery and the lower left heart chamber. If the aortic valve has only two flaps, called cusps, instead of the usual three, it's called a bicuspid valve.
- Subaortic stenosis. This is a narrowing of the area below the aortic valve. It blocks blood flow from the lower left heart chamber to the aorta.
- Patent ductus arteriosus. The ductus arteriosus is a blood vessel that connects the left lung artery to the aorta. When a baby is growing in the womb, this vessel lets blood go around the lungs. Shortly after birth, the ductus arteriosus usually closes. If it stays open, the opening is called a patent ductus arteriosus.
- Holes in the heart. Some people with coarctation of the aorta also are born with a hole in the heart. If the hole is between the upper heart chambers, it is called an atrial septal defect. A hole between the lower heart chambers is called a ventricular septal defect.
- Congenital mitral valve stenosis. This is a type of heart valve disease that some people are born with. The valve between the upper and lower left heart chambers is narrowed. It's harder for blood to move through the valve.
Complications
Complications of coarctation of the aorta happen because the left lower heart chamber has to work harder to pump blood through the narrowed artery. This makes blood pressure go up in the lower left heart chamber. Also, the wall of the chamber can get thick. This condition is called ventricular hypertrophy.
Complications of coarctation of the aorta include:
- Long-term high blood pressure. Blood pressure usually drops after surgery to fix the aorta. But it may still be higher than usual.
- A weakened or bulging artery in the brain, also known as a brain aneurysm.
- Bleeding in the brain.
- A rupture or tear in the body's main artery, called an aortic dissection.
- A bulge in the wall of the body's main artery, called an aortic aneurysm.
- Coronary artery disease.
- Stroke.
Prompt treatment is needed to help prevent complications. Without treatment, coarctation of the aorta may lead to:
- Kidney failure.
- Heart failure.
- Death.
Some people have complications after treatment for coarctation of the aorta. These complications include:
- Re-narrowing of the aorta, called re-coarctation.
- Aortic aneurysm or rupture.
To prevent complications, people with coarctation of the aorta need regular health checkups for life.
Prevention
There's no known way to prevent coarctation of the aorta. Tell your healthcare team if you have a family history of heart conditions present at birth.
Diagnosis
Diagnosis of aortic coarctation may depend on how severe the heart condition is. Severe aortic coarctation is usually diagnosed soon after birth. The condition may be seen on ultrasound images taken during pregnancy.
If the condition is mild, it may not be found until later in life.
To diagnose aortic coarctation, a healthcare professional checks blood pressure in the arms and legs. Depending on which part of the aorta is affected, blood pressure may be high in the arms and low in the legs and ankles. The pulse may be weak or delayed in the legs.
A whooshing sound called a heart murmur may be heard when listening to the heart.
Tests
Tests are done to diagnose coarctation of the aorta.
- Echocardiogram. Sound waves are used to create images of the beating heart. An echocardiogram shows how blood flows through the heart. The test can often tell which part and how much of the aorta is narrowed. An echocardiogram also helps healthcare professionals plan treatment for coarctation of the aorta.
- Electrocardiogram (ECG or EKG). This quick and painless test checks the heartbeat. Sensors called electrodes stick to the chest and sometimes to the arms or legs. Wires connect the sensors to a machine, which displays or prints results. If the aorta is very narrowed, an ECG may show of thickening of the walls of the lower heart chambers.
- Chest X-ray. A chest X-ray shows the condition of the heart and lungs. A chest X-ray might show a narrowing in the aorta at the site of the coarctation.
- Cardiac magnetic resonance imaging (MRI). This test uses magnetic fields and radio waves to create detailed images of the heart and blood vessels. It can show which part and how much of the aorta is narrowed. A healthcare professional also may use MRI results to guide treatment.
- Computerized tomography (CT) scan. A CT scan uses a series of X-rays to create detailed cross-sectional images of the body.
-
Coronary angiogram with cardiac catheterization. A coronary angiogram uses X-rays to look at the heart's blood vessels, called the coronary arteries. It's usually done to see if a blood vessel is narrowed or blocked. A coronary angiogram is part of a general group of heart tests and treatments called cardiac catheterization.
During cardiac catheterization, a thin flexible tube called a catheter is placed in a blood vessel, usually in the groin or wrist, and guided to the heart. Dye flows through the catheter to arteries in the heart. The dye makes the arteries easier to see on X-ray images and video. Cardiac catheterization can help determine how much of the aorta is narrowed.
- CT angiogram. This test looks at the arteries that supply blood to the heart. It uses a powerful X-ray machine to make images of the heart and its blood vessels. A CT angiogram uses a dye and special X-rays to show how blood flows through the veins and arteries. The test can show the location and severity of coarctation of the aorta. It also can tell whether other blood vessels are affected. A CT angiogram also can be used to guide treatment.
Treatment
Treatment for coarctation of the aorta depends on how old the person is when the heart condition is diagnosed. Treatment also depends on how much of the aorta is narrowed.
Coarctation of the aorta treatment may include:
- Medicines.
- A heart procedure.
- Surgery.
If there are other congenital heart defects, they may be repaired at the same time.
Medication
Medicines for aortic coarctation may include:
- Blood pressure medicines. Medicines are used to control blood pressure before repair surgery. Although fixing the aorta can improve blood pressure, many people still need blood pressure medicine after the repair surgery.
- Medicine to keep the ductus arteriosus open. Babies are born with a temporary opening called the ductus arteriosus between the aorta and the pulmonary artery. This opening lets some blood go to the lungs. The ductus arteriosus most often closes soon after birth. But medicine can keep it open. Babies with severe coarctation of the aorta often get such medicine until surgery is done to fix the aorta.
Surgery or other procedures
Surgery or a heart procedure can be done to repair aortic coarctation. Options include:
-
Balloon angioplasty and stenting. This may be the first treatment for aortic coarctation. Sometimes it's done if the aorta gets narrow again after coarctation surgery. The treatment helps widen a narrowed artery and improve blood flow.
During angioplasty, a doctor uses a thin tube called a catheter and a tiny balloon to open a narrowed artery. Usually, a small metal coil called a stent is placed in the artery. The stent keeps the artery open. It also reduces the risk of renarrowing.
- Resection with end-to-end anastomosis. A surgeon removes the narrowed area of the aorta. This is called a resection. The surgeon then connects the two healthy parts of the aorta. This is called anastomosis.
- Subclavian flap aortoplasty. A surgeon takes part of the blood vessel that delivers blood to the left arm, called the left subclavian artery, and uses it to widen the narrowed area of the aorta.
- Bypass graft repair. This surgery uses a tube called a graft to create a new path for blood to flow around the narrowed area of the aorta.
- Patch aortoplasty. The surgeon cuts across the narrowed area of the aorta and patches in a piece of material to expand the blood vessel. This treatment is useful if the coarctation involves a long part of the aorta.
After aortic repair surgery, health checkups are needed for life to keep track of blood pressure and watch for complications.
Lifestyle and home remedies
People who had coarctation of the aorta need to take steps to control blood pressure and watch for complications. Follow these tips:
- Get regular exercise. Regular exercise helps lower blood pressure. Talk with your healthcare team about the amount and type of exercise that's best for you. Some physical activities, such as weight lifting, can temporarily raise blood pressure.
- Talk with your healthcare team before getting pregnant. Coarctation of the aorta, even after it's fixed, may increase the risk of an aortic tear or rupture during pregnancy and childbirth. Before becoming pregnant, talk with a doctor trained in congenital heart diseases, called an adult congenital cardiologist. Together you can go over the possible risks and complications.
- Prevent heart infections. Bacteria can affect the inner lining of the heart or valves, causing an infection called endocarditis. People with some heart conditions may need to take antibiotics before dental work to prevent this infection. Ask your healthcare professional whether you need preventive antibiotics.
Preparing for an appointment
If coarctation of the aorta is diagnosed at birth, there may not be time to prepare. If symptoms aren't noticed until later in life, see a doctor trained in heart problems present at birth. This type of healthcare professional is called a congenital cardiologist.
Here's some information to help you prepare for the appointment.
What you can do
Write down the following and bring the notes with you to your appointment:
- Any symptoms, including any that may seem unrelated to coarctation of the aorta. Note when each symptom began.
- Important medical information, including any family history of heart problems present at birth.
- All medicines, vitamins and supplements taken during pregnancy or currently taken. Include the doses.
- Any questions you want to ask your healthcare professional.
Questions to ask the healthcare professional include:
- How is coarctation of the aorta treated?
- What treatment do you recommend and why?
- What will be involved in recovery and rehabilitation after surgery?
- How often are followup tests and checkups needed?
- What is the risk of complications from this condition?
- What symptoms or warning signs should I watch for at home?
- What is the long-term outlook?
- Do you recommend any diet, exercise or sports restrictions?
- Are antibiotics needed before dental work or other medical procedures?
- Is pregnancy safe for those with coarctation of the aorta?
- What is the risk that my or my child's future children will have coarctation of the aorta?
Don't hesitate to ask any other questions.
Also ask someone to go with you to the appointment, if possible. Someone who goes with you can help remember what the health professional says.
What to expect from your doctor
Your healthcare team is likely to ask you many questions. Being ready to answer them may save time to go over anything you want to spend more time on. Your healthcare team may ask:
- When did you first notice your child's symptoms?
- Can you describe your child's symptoms?
- Does your child have any breathing problems, such as running out of breath easily or breathing rapidly?
- Does your child tire easily?
- Does your child sweat heavily?
- Does your child seem irritable?
- Do your child's symptoms include chest pain?
- Does your child often have cold feet?
- When do these symptoms occur?
- Do the symptoms come and go, or does your child always have them?
- Do the symptoms seem to be getting worse?
- Do you have a family history of congenital heart defects?
- Does anything make your child's symptoms better?
If you had coarctation of the aorta, your healthcare team may ask:
- When did the symptoms start?
- Have the symptoms gotten worse over time?
- Does exercise or activity make your symptoms worse?
- Have you been diagnosed with any other medical conditions?
- Do you have a family history of heart problems?
- Are you planning to become pregnant in the future?
© 1998-2026 Mayo Foundation for Medical Education and Research(MFMER). All rights reserved. Terms of Use
