Dysphagia
Conditions
Overview
Dysphagia is a medical term for difficulty swallowing. Dysphagia can be a painful condition. In some cases, swallowing is impossible.
Occasional difficulty swallowing, such as when you eat too fast or don't chew your food well enough, usually isn't cause for concern. But ongoing dysphagia can be a serious medical condition that needs treatment.
Dysphagia can happen at any age, but it's more common in older adults. The causes of swallowing problems vary, and treatment depends on the cause.
Symptoms
Symptoms associated with dysphagia can include:
- Pain while swallowing.
- Not being able to swallow.
- Feeling as if food is stuck in the throat or chest or behind the breastbone.
- Drooling.
- Hoarseness.
- Food coming back up, called regurgitation.
- Frequent heartburn.
- Food or stomach acid backing up into the throat.
- Weight loss.
- Coughing or gagging when swallowing.
When to see a doctor
See a healthcare professional if you regularly have difficulty swallowing or if weight loss, regurgitation or vomiting happens with your dysphagia.
If a blockage makes it hard to breathe, call for emergency help immediately. If you're unable to swallow because you feel that food is stuck in your throat or chest, go to the nearest emergency department.
Causes
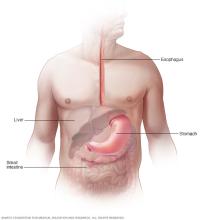
Swallowing is complex, involving many muscles and nerves. Any condition that weakens or damages these muscles and nerves or causes narrowing of the back of the throat or esophagus can cause dysphagia.
Dysphagia generally falls into one of the following categories.
Esophageal dysphagia
Esophageal dysphagia refers to the sensation of food sticking or getting caught in the base of the throat or in the chest after swallowing begins. Some causes of esophageal dysphagia include:
- Achalasia. Achalasia is a condition that leads to trouble swallowing. Damaged nerves or muscles make it hard for the esophagus to squeeze food and liquid into the stomach. Achalasia tends to worsen over time.
- Esophageal spasm. This condition causes high-pressure, poorly coordinated contractions of the esophagus, usually after swallowing. Esophageal spasm affects the involuntary muscles in the walls of the lower esophagus.
- A narrowed esophagus. Known as a stricture, a narrowed esophagus can trap large pieces of food. Tumors or scar tissue, often caused by gastroesophageal reflux disease (GERD), can cause narrowing.
- Esophageal tumors. Difficulty swallowing tends to get progressively worse when esophageal tumors are present. Growing tumors steadily narrow the esophagus.
- Foreign bodies. Sometimes food or another object can partially block the throat or esophagus. Older adults with dentures and people who have difficulty chewing their food may be more likely to have a piece of food become stuck in the throat or esophagus.
- Esophageal ring. A thin area of narrowing in the lower esophagus can occasionally cause difficulty swallowing solid foods.
- GERD. Stomach acid backing up into the esophagus can damage esophageal tissues. This can lead to spasm or scarring and narrowing of the lower esophagus.
- Eosinophilic esophagitis. Eosinophilic esophagitis is a disease of the immune system. It is caused when white blood cells, called eosinophils, build up in the esophagus.
- Scleroderma. Scleroderma causes the development of scar-like tissue, resulting in stiffening and hardening of tissues. This can weaken the lower esophageal sphincter. As a result, acid backs up into the esophagus and causes frequent heartburn.
- Radiation therapy. This cancer treatment can lead to inflammation and scarring of the esophagus.
Oropharyngeal dysphagia
Certain conditions can weaken the throat muscles, making it difficult to move food from the mouth into the throat and esophagus during swallowing. A person might choke, gag or cough when trying to swallow, or have the sensation of food or fluids going down the windpipe, called the trachea, or up the nose. This can lead to pneumonia.
Causes of oropharyngeal dysphagia include:
- Neurological disorders. Certain disorders — such as multiple sclerosis, muscular dystrophy and Parkinson's disease — can cause dysphagia.
- Neurological damage. Sudden neurological damage, such as from a stroke or a brain or spinal cord injury, can affect the ability to swallow.
- Pharyngoesophageal diverticulum, also known as Zenker diverticulum. A small pouch, known as a diverticulum, that forms and collects food particles in the throat, often just above the esophagus, leads to difficulty swallowing, gurgling sounds, bad breath, and repeated throat clearing or coughing.
- Cancer. Certain cancers and some cancer treatments, such as radiation, can cause difficulty swallowing.
Risk factors
The following are risk factors for dysphagia:
- Aging. Older adults are at higher risk of swallowing difficulties. This is due to natural aging and wear and tear on the esophagus as well as a greater risk of certain conditions, such as stroke or Parkinson's disease. But dysphagia isn't considered a typical sign of aging.
- Certain health conditions. People with certain neurological or nervous system disorders are more likely to have difficulty swallowing.
Complications
Difficulty swallowing can lead to:
- Malnutrition, weight loss and dehydration. Dysphagia can make it difficult to take in enough food and fluids.
- Aspiration pneumonia. Food or liquid entering the airway during attempts to swallow can cause aspiration pneumonia as a result of the food introducing bacteria into the lungs.
- Choking. Food stuck in the throat can cause choking. If food completely blocks the airway and no one intervenes with a successful Heimlich maneuver, death can occur.
Prevention
Although swallowing difficulties can't be prevented, you can reduce your risk of occasional difficulty swallowing by eating slowly and chewing your food well. However, if you have symptoms of dysphagia, see a healthcare professional.
If you have GERD, see a healthcare professional for treatment.
Diagnosis
A member of your healthcare team will likely ask you for a description and history of your swallowing difficulties, perform a physical exam, and use various tests to find the cause of your swallowing problem.
Tests can include:
-
X-ray with a contrast material, called a barium X-ray. You drink a barium solution that coats the esophagus, making it easier to see on X-rays. A healthcare team can then see changes in the shape of the esophagus and can check the muscular activity.
You also may be asked to swallow solid food or a pill coated with barium. This allows the healthcare team to watch the muscles in the throat during swallowing or to look for blockages in the esophagus that the liquid barium solution might not show.
- Dynamic swallowing study. This study involves swallowing barium-coated foods of different consistencies. It provides an image of these foods as they travel down the throat. The images might show problems in the coordination of the mouth and throat muscles during swallowing. The images also can show if food is going into the breathing tube.
- Endoscopy. Endoscopy involves passing a thin, flexible lighted instrument, called an endoscope, down the throat. This allows your healthcare team to see your esophagus. Tissue samples, called biopsies, may be collected. The samples are studied to look for inflammation, eosinophilic esophagitis, narrowing or a tumor.
- Fiber-optic endoscopic evaluation of swallowing (FEES). During a FEES study, a healthcare professional examines the throat with an endoscope during swallowing.
- Esophageal muscle test, called manometry. In manometry (muh-NOM-uh-tree), a small tube is inserted into the esophagus and connected to a pressure recorder to measure the muscle contractions of the esophagus during swallowing.
- Imaging scans. These can include a CT scan or an MRI scan. A CT scan combines a series of X-ray views and computer processing to create cross-sectional images of the body's bones and soft tissues. An MRI scan uses a magnetic field and radio waves to create detailed images of organs and tissues.
Treatment
Treatment for dysphagia depends on the type or cause of your swallowing disorder.
Oropharyngeal dysphagia
For oropharyngeal dysphagia, you may be referred to a speech or swallowing therapist. Therapy might include:
- Learning exercises. Certain exercises might help coordinate your swallowing muscles or restimulate the nerves that trigger the swallowing reflex.
- Learning swallowing techniques. You also might learn ways to place food in your mouth or position your body and head to help you swallow. Exercises and new swallowing techniques might help if your dysphagia is caused by neurological problems such as Alzheimer's disease or Parkinson's disease.
Esophageal dysphagia
Treatment approaches for esophageal dysphagia might include:
- Esophageal dilation. Dilation involves placing an endoscope into the esophagus and inflating an attached balloon to stretch it. This treatment is used for achalasia, esophageal stricture, motility disorders, or an irregular ring of tissue at the junction of the esophagus and stomach, known as Schatzki ring. Long, flexible tubes of varying diameter also may be inserted through the mouth into the esophagus to treat strictures and rings.
- Surgery. For an esophageal tumor, achalasia or pharyngoesophageal diverticulum, you might need surgery to clear your esophageal path.
-
Medicines. Difficulty swallowing caused by GERD can be treated with prescription medicines to reduce stomach acid. You might need to take these medicines for a long time.
Corticosteroids might be recommended for eosinophilic esophagitis. For esophageal spasm, smooth muscle relaxants might help.
- Diet. You may be prescribed a special diet to help with your symptoms depending on the cause of the dysphagia. If you have eosinophilic esophagitis, diet might be used as treatment.
Severe dysphagia
If difficulty swallowing prevents you from eating and drinking enough and treatment doesn't allow you to swallow safely, a feeding tube may be recommended. A feeding tube provides nutrients without the need to swallow.
Surgery
Surgery might be needed to relieve swallowing problems caused by throat narrowing or blockages. Blockages include bony outgrowths, vocal cord paralysis, pharyngoesophageal diverticula, GERD and achalasia. Surgery also can treat esophageal cancer. Speech and swallowing therapy is usually helpful after surgery.
The type of surgical treatment depends on the cause of dysphagia. Some examples are:
- Laparoscopic Heller myotomy. This involves cutting the muscle at the lower end of the esophagus, called the esophageal sphincter. In people who have achalasia, the esophageal sphincter fails to open and release food into the stomach. Heller myotomy helps correct this problem.
- Peroral endoscopic myotomy (POEM). The POEM procedure involves creating an incision in the inside lining of the esophagus to treat achalasia. Then, as in a Heller myotomy, the surgeon or gastroenterologist cuts the muscle at the lower end of the esophageal sphincter.
- Stent placement. A metal or plastic tube called a stent may be used to prop open a narrowed or blocked esophagus. Some stents are permanent, such as those for people with esophageal cancer, while others are removed later.
- OnabotulinumtoxinA (Botox). This can be injected into the muscle at the end of the esophagus, called the esophageal sphincter. This causes it to relax, improving swallowing in achalasia. Less invasive than surgery, this technique might require repeat injections. More study is needed.
Lifestyle and home remedies
If you have trouble swallowing, be sure to see a healthcare professional. You also may try these approaches to help ease symptoms:
- Changing your eating habits. Try eating smaller, more frequent meals. Cut your food into smaller pieces, chew food thoroughly and eat more slowly. If you have difficulty swallowing liquids, there are products you can buy to thicken liquids.
- Trying foods with different textures to see if some cause you more trouble. Thin liquids, such as coffee and juice, are a problem for some people, and sticky foods, such as peanut butter or caramel, can make swallowing difficult. Avoid foods that cause you trouble.
- Limiting alcohol and caffeine. These can dry your mouth and throat, making swallowing more difficult.
Preparing for an appointment
See a healthcare professional if you're having problems swallowing. Depending on the suspected cause, you may be referred to an ear, nose and throat specialist; a doctor who specializes in treating digestive disorders, called a gastroenterologist; or a doctor who specializes in diseases of the nervous system, called a neurologist.
Here's some information to help you prepare for your appointment.
What you can do
When you make the appointment, ask if there's anything you need to do in advance, such as restrict your diet.
Make a list of:
- Your symptoms, including any that seem unrelated to the reason for which you scheduled the appointment, and when they began.
- Key personal information, including major stresses or recent life changes.
- All medicines, vitamins and supplements you take, including doses.
- Questions to ask your healthcare team.
For dysphagia, questions to ask include:
- What's the likeliest cause of my symptoms?
- What are other possible causes?
- What tests do I need?
- Is this condition temporary or long lasting?
- I have other health conditions. How can I best manage them together?
- Do I need to restrict my diet?
- Are there brochures or other printed material I can have? What websites do you recommend?
What to expect from your doctor
Your healthcare team is likely to ask you a number of questions, including:
- Have your symptoms been continuous or occasional?
- Does anything seem to improve your symptoms?
- What, if anything, appears to worsen your symptoms? For example, are certain foods harder to swallow than others?
- Do you have difficulty swallowing solids, liquids or both?
- Do you cough or gag when you try to swallow?
- Did you first have trouble swallowing solids and then develop difficulty swallowing liquids?
- Do you bring food back up after swallowing it?
- Do you ever vomit or bring up blood or black material?
- Have you lost weight?
What you can do in the meantime
Until your appointment, it might help to chew your food more slowly and thoroughly than usual. If you have heartburn or GERD, try eating smaller meals and not eating right before bedtime. Antacids that you can get without a prescription also might help temporarily.
© 1998-2026 Mayo Foundation for Medical Education and Research(MFMER). All rights reserved. Terms of Use
