Edema
Conditions
Overview
Edema is swelling caused by too much fluid trapped in the body's tissues. Edema can affect any part of the body. But it's more likely to show up in the legs and feet.
Medicines and pregnancy can cause edema. It also can be the result of a disease, such as congestive heart failure, kidney disease, venous insufficiency or cirrhosis of the liver.
Wearing compression garments and reducing salt in the diet often relieves edema. When a disease causes edema, the disease needs treatment, as well.
Symptoms
Symptoms of edema include:
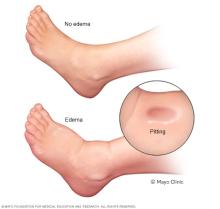
- Swelling or puffiness of the tissue right under the skin, especially in legs or arms.
- Stretched or shiny skin.
- Skin that holds a dimple, also known as pitting, after it's been pressed for a few seconds.
- Swelling of the belly, also called the abdomen, so that it's bigger than usual.
- Feeling of leg heaviness.
When to see a doctor
Make an appointment to see a health care provider for swelling, stretched or shiny skin, or skin that holds a dimple after being pressed. See a provider right away for:
- Shortness of breath.
- Irregular heartbeat.
- Chest pain.
These can be signs of fluid buildup in the lungs, also known as pulmonary edema. It can be life-threatening and needs quick treatment.
After sitting for a long time, such as on a long flight, call your care provider if you get leg pain and swelling that won't go away. Especially if the pain and swelling is on one side, these can be symptoms of a blood clot deep in the vein, also known as deep vein thrombosis, or DVT.
Causes
Edema occurs when tiny blood vessels in the body, also known as capillaries, leak fluid. The fluid builds up in nearby tissues. The leak leads to swelling.
Causes of mild cases of edema include:
- Sitting or staying in one position for too long.
- Eating too much salty food.
- Being premenstrual.
- Being pregnant.
Edema also can be a side effect of some medicines. These include:
- High blood pressure medicines.
- Nonsteroidal anti-inflammatory medicines.
- Steroid medicines.
- Estrogens.
- Certain diabetes medicines called thiazolidinediones.
- Medicines use to treat nerve pain.
Sometimes edema can be a sign of a more serious condition. Illnesses that can cause edema include:
-
Congestive heart failure. Congestive heart failure causes one or both of the heart's lower chambers stop pumping blood well. As a result, blood can back up in the legs, ankles and feet, causing edema.
Congestive heart failure can also cause swelling in the stomach area. This condition also can cause fluid to build up in the lungs. Known as pulmonary edema, this can lead to shortness of breath.
- Liver damage. This liver damage from cirrhosis can cause fluid to build up in the stomach area. and in the legs. This fluid buildup in the stomach area is known as ascites.
- Kidney disease. Kidney disease can cause fluid and salts in the blood to build up. Edema linked to kidney disease usually occurs in the legs and around the eyes.
- Kidney damage. Damage to the tiny, filtering blood vessels in the kidneys can result in nephrotic syndrome. In nephrotic syndrome, decreased levels of protein in the blood can lead to edema.
- Weakness or damage to veins in your legs. This condition, known as chronic venous insufficiency, harms the one-way valves in the leg. One-way valves keep blood flowing in one direction. Damage to the valves allows blood to pool in the leg veins and causes swelling.
- Deep vein thrombosis, also called DVT. Sudden swelling in one leg with pain in the calf muscle can be due to a blood clot in one of the leg veins. DVT requires medical help right away.
- Problems with the system in the body that clears extra fluid from tissues. If the body's lymphatic system is damaged, such as by cancer surgery, the lymphatic system might not drain well.
- Severe, long-term lack of protein. An extreme lack of protein in the diet over time can lead to edema.
Risk factors
The following increases the risk of edema:
- Being pregnant.
- Taking certain medicines.
- Having a long-lasting illness, such as congestive heart failure or liver or kidney disease.
- Having surgery that involves a lymph node.
Complications
If left untreated, edema can cause:
- Swelling that gets more and more painful.
- Problems walking.
- Stiffness.
- Stretched skin, which can itch.
- Increased risk of infection in the swollen area.
- Scarring between layers of tissue.
- Less blood flow.
- Less ability of the of arteries, veins, joints and muscles to stretch.
- Increased risk of skin ulcers.
Diagnosis
To understand the cause of your edema, a health care provider will do a physical exam and ask about your medical history. This might be enough to figure out the cause. Sometimes, diagnosis might require blood tests, ultrasound exams, vein studies or others.
Treatment
Mild edema usually goes away on its own. Wearing compression garments and raising the affected arm or leg higher than the heart helps.
Medicines that help the body get rid of too much fluid through urine can treat worse forms of edema. One of the most common of these water pills, also known as diuretics, is furosemide (Lasix). A health care provider can decide about the need for water pills.
Treating the cause of the swelling is often the focus over time. If edema is a result of medicines, for example, a care provider might change the dose or look for another medicine that doesn't cause edema.
Lifestyle and home remedies

The following may help decrease edema and keep it from coming back. Talk to your health care provider about which of these might help you.
-
Use pressure. If edema affects an arm or leg, wearing compression stockings, sleeves or gloves might help. These garments keep pressure on the limbs to prevent fluid from building up. Usually worn after the swelling goes down, they help prevent more swelling.
For pregnant people, wearing support stockings during air travel might help.
- Move. Moving and using the muscles in the part of the body that's swollen, especially the legs, might help move fluid back toward the heart. A health care provider can talk about exercises that might reduce swelling.
- Raise. Hold the swollen part of the body above the level of the heart several times a day. Sometimes, raising the swollen area during sleep can be helpful.
- Massage. Stroking the affected area toward the heart using firm, but not painful, pressure might help move fluid out of that area.
- Protect. Keep the swollen area clean and free from injury. Use lotion or cream. Dry, cracked skin is more open to scrapes, cuts and infection. Always wear socks or shoes on the feet if that's where the swelling usually is.
- Reduce salt. A health care provider can talk about limiting salt. Salt can increase fluid buildup and worsen edema.
Preparing for an appointment
Unless you're already seeing a health care provider for a condition such as pregnancy, you'll probably start by seeing your family provider.
Here's some information to help you get ready for your appointment.
What you can do
- Be aware of anything you need to do before the appointment. When you make the appointment ask if there's anything you need to do to prepare. For example, you might need to fast before certain tests.
- Write down your symptoms, including any that may seem like they have nothing to do with the reason for which you made the appointment. Note when the symptoms began.
- Make a list of your key medical information, such as other conditions you have. List medicines, vitamins and supplements you take, including doses.
- Make a list of questions to ask your provider. Bring something to write with or a recorder to get down the answers.
- Take pictures on your phone. If swelling gets much worse at night, it might help your health care provider to see how bad it gets.
For edema, some questions to ask might include:
- What are the possible causes of my symptoms?
- What tests do I need? How do I prepare for them?
- Is my condition long-lasting or temporary?
- What treatments, if any, do you recommend?
- I have other medical problems. How do I manage these conditions together?
- Do you have brochures or other printed material I can have? What websites do you recommend?
What to expect from your doctor
Your provider is likely to ask you questions, such as:
- Do your symptoms come and go, or are they always there?
- Have you had edema before?
- Are you short of breath?
- Does anything seem to make your symptoms better?
- Is there less swelling after a night's rest?
- Does anything make your symptoms worse?
- What kinds of foods do you regularly eat?
- Do you restrict salt and salty foods?
- Do you drink alcohol?
- Are you urinating as usual?
© 1998-2026 Mayo Foundation for Medical Education and Research(MFMER). All rights reserved. Terms of Use
