Knee pain
Conditions
Overview
Knee pain is a common complaint that affects people of all ages. Knee pain may be the result of an injury, such as a ruptured ligament or torn cartilage. Medical conditions — including arthritis, gout and infections — also can cause knee pain.
Many types of minor knee pain respond well to self-care measures. Physical therapy and knee braces also can help relieve pain. In some cases, however, your knee may require surgical repair.
Symptoms
The location and severity of knee pain may vary, depending on the cause of the problem. Signs and symptoms that sometimes accompany knee pain include:
- Swelling and stiffness
- Redness and warmth to the touch
- Weakness or instability
- Popping or crunching noises
- Inability to fully straighten the knee
When to see a doctor
Call your doctor if you:
- Can't bear weight on your knee or feel as if your knee is unstable or gives out
- Have marked knee swelling
- Are unable to fully extend or flex your knee
- See an obvious deformity in your leg or knee
- Have a fever, in addition to redness, pain and swelling in your knee
- Have severe knee pain that is associated with an injury
Causes

Knee pain can be caused by injuries, mechanical problems, types of arthritis and other problems.
Injuries
A knee injury can affect any of the ligaments, tendons or fluid-filled sacs (bursae) that surround your knee joint as well as the bones, cartilage and ligaments that form the joint itself. Some of the more common knee injuries include:
- ACL injury. An ACL injury is a tear of the anterior cruciate ligament (ACL) — one of four ligaments that connect your shinbone to your thighbone. An ACL injury is particularly common in people who play basketball, soccer or other sports that require sudden changes in direction.
- Fractures. The bones of the knee, including the kneecap (patella), can be broken during falls or auto accidents. Also, people whose bones have been weakened by osteoporosis can sometimes sustain a knee fracture simply by stepping wrong.
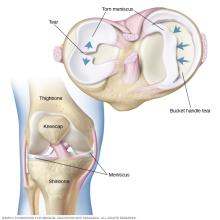
- Torn meniscus. The meniscus is the tough, rubbery cartilage that acts as a shock absorber between your shinbone and thighbone. It can be torn if you suddenly twist your knee while bearing weight on it.
- Knee bursitis. Some knee injuries cause inflammation in the bursae, the small sacs of fluid that cushion the outside of your knee joint so that tendons and ligaments glide smoothly over the joint.
- Patellar tendinitis. Tendinitis causes irritation and inflammation of one or more tendons — the thick, fibrous tissues that attach muscles to bones. This inflammation can happen when there's an injury to the patellar tendon, which runs from the kneecap (patella) to the shinbone and allows you to kick, run and jump. Runners, skiers, cyclists, and those involved in jumping sports and activities may develop patellar tendinitis.
Mechanical problems
Some examples of mechanical problems that can cause knee pain include:
- Loose body. Sometimes injury or degeneration of bone or cartilage can cause a piece of bone or cartilage to break off and float in the joint space. This may not create any problems unless the loose body interferes with knee joint movement, in which case the effect is something like a pencil caught in a door hinge.
- Iliotibial band syndrome. This occurs when the tough band of tissue that extends from the outside of your hip to the outside of your knee (iliotibial band) becomes so tight that it rubs against the outer portion of your thighbone. Distance runners and cyclists are especially susceptible to iliotibial band syndrome.
- Dislocated kneecap. This occurs when the triangular bone that covers the front of your knee (patella) slips out of place, usually to the outside of your knee. In some cases, the kneecap may stay displaced and you'll be able to see the dislocation.
- Hip or foot pain. If you have hip or foot pain, you may change the way you walk to spare your painful joint. But this altered gait can place more stress on your knee joint and cause knee pain.
Types of arthritis
More than 100 different types of arthritis exist. The varieties most likely to affect the knee include:
- Osteoarthritis. Sometimes called degenerative arthritis, osteoarthritis is the most common type of arthritis. It's a wear-and-tear condition that occurs when the cartilage in your knee deteriorates with use and age.
- Rheumatoid arthritis. The most debilitating form of arthritis, rheumatoid arthritis is an autoimmune condition that can affect almost any joint in your body, including your knees. Although rheumatoid arthritis is a chronic disease, it tends to vary in severity and may even come and go.
- Gout. This type of arthritis occurs when uric acid crystals build up in the joint. While gout most commonly affects the big toe, it can also occur in the knee.
- Pseudogout. Often mistaken for gout, pseudogout is caused by calcium-containing crystals that develop in the joint fluid. Knees are the most common joint affected by pseudogout.
- Septic arthritis. Sometimes your knee joint can become infected, leading to swelling, pain and redness. Septic arthritis often occurs with a fever, and there's usually no trauma before the onset of pain. Septic arthritis can quickly cause extensive damage to the knee cartilage. If you have knee pain with any of the symptoms of septic arthritis, see your doctor right away.
Other problems
Patellofemoral pain syndrome is a general term that refers to pain arising between the kneecap and the underlying thighbone. It's common in athletes; in young adults, especially those whose kneecap doesn't track properly in its groove; and in older adults, who usually develop the condition as a result of arthritis of the kneecap.
Risk factors
A number of factors can increase your risk of having knee problems, including:
- Excess weight. Being overweight or obese increases stress on your knee joints, even during ordinary activities such as walking or going up and down stairs. It also puts you at increased risk of osteoarthritis by accelerating the breakdown of joint cartilage.
- Lack of muscle flexibility or strength. A lack of strength and flexibility can increase the risk of knee injuries. Strong muscles help stabilize and protect your joints, and muscle flexibility can help you achieve full range of motion.
- Certain sports or occupations. Some sports put greater stress on your knees than do others. Alpine skiing with its rigid ski boots and potential for falls, basketball's jumps and pivots, and the repeated pounding your knees take when you run or jog all increase your risk of knee injury. Jobs that require repetitive stress on the knees such as construction or farming also can increase your risk.
- Previous injury. Having a previous knee injury makes it more likely that you'll injure your knee again.
Complications
Not all knee pain is serious. But some knee injuries and medical conditions, such as osteoarthritis, can lead to increasing pain, joint damage and disability if left untreated. And having a knee injury — even a minor one — makes it more likely that you'll have similar injuries in the future.
Prevention
Although it's not always possible to prevent knee pain, the following suggestions may help ward off injuries and joint deterioration:
- Keep extra pounds off. Maintain a healthy weight; it's one of the best things you can do for your knees. Every extra pound puts additional strain on your joints, increasing the risk of injuries and osteoarthritis.
- Be in shape to play your sport. To prepare your muscles for the demands of sports participation, take time for conditioning.
- Practice perfectly. Make sure the technique and movement patterns you use in your sports or activity are the best they can be. Lessons from a professional can be very helpful.
-
Get strong, stay flexible. Weak muscles are a leading cause of knee injuries. You'll benefit from building up your quadriceps and hamstrings, the muscles on the front and back of your thighs that help support your knees. Balance and stability training helps the muscles around your knees work together more effectively.
And because tight muscles also can contribute to injury, stretching is important. Try to include flexibility exercises in your workouts.
- Be smart about exercise. If you have osteoarthritis, chronic knee pain or recurring injuries, you may need to change the way you exercise. Consider switching to swimming, water aerobics or other low-impact activities — at least for a few days a week. Sometimes simply limiting high-impact activities will provide relief.
Diagnosis
During the physical exam, your doctor is likely to:
- Inspect your knee for swelling, pain, tenderness, warmth and visible bruising
- Check to see how far you can move your lower leg in different directions
- Push on or pull the joint to evaluate the integrity of the structures in your knee
Imaging tests
In some cases, your doctor might suggest tests such as:
- X-ray. Your doctor may first recommend having an X-ray, which can help detect bone fractures and degenerative joint disease.
- Computerized tomography (CT) scan. CT scanners combine X-rays taken from many different angles to create cross-sectional images of the inside of your body. CT scans can help diagnose bone problems and subtle fractures. A special kind of CT scan can accurately identify gout even when the joint is not inflamed.
- Ultrasound. This technology uses sound waves to produce real-time images of the soft tissue structures within and around your knee. Your doctor may want to move your knee into different positions during the ultrasound to check for specific problems.
- Magnetic resonance imaging (MRI). An MRI uses radio waves and a powerful magnet to create 3D images of the inside of your knee. This test is particularly useful in revealing injuries to soft tissues such as ligaments, tendons, cartilage and muscles.
Lab tests
If your doctor suspects an infection or inflammation, you're likely to have blood tests and sometimes a procedure called arthrocentesis, in which a small amount of fluid is removed from within your knee joint with a needle and sent to a laboratory for analysis.
Treatment
Treatments will vary, depending upon what exactly is causing your knee pain.
Medications
Your doctor may prescribe medications to help relieve pain and to treat the conditions causing your knee pain, such as rheumatoid arthritis or gout.
Therapy
Strengthening the muscles around your knee will make it more stable. Your doctor may recommend physical therapy or different types of strengthening exercises based on the specific condition that is causing your pain.
If you are physically active or practice a sport, you may need exercises to correct movement patterns that may be affecting your knees and to establish good technique during your sport or activity. Exercises to improve your flexibility and balance also are important.
Arch supports, sometimes with wedges on one side of the heel, can help shift pressure away from the side of the knee most affected by osteoarthritis. In certain conditions, different types of braces may be used to help protect and support the knee joint.
Injections
In some cases, your doctor may suggest injecting medications or other substances directly into your joint. Examples include:
- Corticosteroids. Injections of a corticosteroid drug into your knee joint may help reduce the symptoms of an arthritis flare and provide pain relief that may last a few months. These injections aren't effective in all cases.
- Hyaluronic acid. A thick fluid, similar to the fluid that naturally lubricates joints, hyaluronic acid can be injected into your knee to improve mobility and ease pain. Although study results have been mixed about the effectiveness of this treatment, relief from one or a series of shots may last as long as six months.
- Platelet-rich plasma (PRP). PRP contains a concentration of many different growth factors that appear to reduce inflammation and promote healing. Some studies have found that PRP may benefit certain people with osteoarthritis, but more studies are needed.
Surgery
If you have an injury that may require surgery, it's usually not necessary to have the operation immediately. Before making a decision, consider the pros and cons of both nonsurgical rehabilitation and surgical reconstruction in relation to what's most important to you. If you choose to have surgery, your options may include:
- Arthroscopic surgery. Depending on your injury, your doctor may be able to examine and repair your joint damage using a fiber-optic camera and long, narrow tools inserted through just a few small incisions around your knee. Arthroscopy may be used to remove loose bodies from your knee joint, remove or repair damaged cartilage (especially if it is causing your knee to lock), and reconstruct torn ligaments.
- Partial knee replacement surgery. In this procedure, your surgeon replaces only the most damaged portion of your knee with parts made of metal and plastic. The surgery can usually be performed through small incisions, so you're likely to heal more quickly than you are with surgery to replace your entire knee.
- Total knee replacement. In this procedure, your surgeon cuts away damaged bone and cartilage from your thighbone, shinbone and kneecap, and replaces it with an artificial joint made of metal alloys, high-grade plastics and polymers.
- Osteotomy. This procedure involves removing bone from the thighbone or shinbone to better align the knee and relieve arthritis pain. This surgery may help you delay or avoid total knee replacement surgery.
Lifestyle and home remedies
Over-the-counter medications — such as ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve) — may help ease knee pain.
Some people find relief by rubbing the affected knee with creams containing a numbing agent, such as lidocaine, or capsaicin, the substance that makes chili peppers hot.
Self-care measures for an injured knee include:
- Rest. Take a break from your normal activities to reduce repetitive strain on your knee, give the injury time to heal and help prevent further damage. A day or two of rest may be all you need for a minor injury. More severe damage is likely to need a longer recovery time.
- Ice. Ice reduces both pain and inflammation. A bag of frozen peas works well because it covers your whole knee. You also can use an ice pack wrapped in a thin towel to protect your skin. Although ice therapy is generally safe and effective, don't use ice for longer than 20 minutes at a time because of the risk of damage to your nerves and skin.
- Heat. You may experience temporary pain relief by applying a heat pack or hot-water bottle to the painful area on your knee.
- Compression. This helps prevent fluid buildup in damaged tissues and maintains knee alignment and stability. Look for a compression bandage that's lightweight, breathable and self-adhesive. It should be tight enough to support your knee without interfering with circulation.
- Elevation. To help reduce swelling, try propping your injured leg on pillows or sitting in a recliner.
Alternative medicine
Research suggests that acupuncture may help relieve knee pain caused by osteoarthritis. Acupuncture involves the placement of hair-thin needles into your skin at specific places on your body.
Preparing for an appointment
You're likely to start by seeing your family doctor. Depending on the cause of your problem, he or she may refer you to a doctor specializing in joint diseases (rheumatologist), joint surgery (orthopedic surgeon) or sports medicine.
What you can do
Before your appointment, you may want to write a list of answers to the following questions:
- When did you begin experiencing symptoms?
- Did a specific injury make your knee start to hurt?
- Have your symptoms been continuous or occasional?
- How severe are your symptoms?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
- What medications and supplements do you take regularly?
What to expect from your doctor
Your doctor may ask some of the following questions:
- Do you exercise or play sports?
- Was the pain caused by an injury?
- Do you experience any swelling, instability or locking of the knee?
- Are you experiencing symptoms in other areas, or just in your knee?
- Have you ever had knee pain before? If so, do you know what the cause was?
© 1998-2026 Mayo Foundation for Medical Education and Research(MFMER). All rights reserved. Terms of Use
