Legg-Calve-Perthes disease
Conditions
Overview
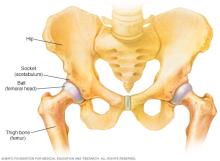
Legg-Calve-Perthes (LEG-kahl-VAY-PER-tuz) disease is a childhood condition that occurs when blood supply to the ball part (femoral head) of the hip joint is temporarily interrupted and the bone begins to die.
This weakened bone gradually breaks apart and can lose its round shape. The body eventually restores blood supply to the ball, and the ball heals. But if the ball is no longer round after it heals, it can cause pain and stiffness. The complete process of bone death, fracture and renewal can take several years.
To keep the ball part of the joint as round as possible, doctors use a variety of treatments that keep it snug in the socket portion of the joint. The socket acts as a mold for the fragmented femoral head as it heals.
Symptoms
Symptoms of Perthes disease include:
- Limping.
- Pain or stiffness in the hip, groin, thigh or knee.
- Limited range of motion of the hip joint.
- Pain that worsens with activity and improves with rest.
Perthes disease usually involves just one hip. Both hips can be affected, but they usually are affected at different times.
When to see a doctor
Make an appointment with your healthcare professional if your child begins limping or complains of hip, groin or knee pain. If your child has a fever or can't bear weight on the leg, seek emergency medical care.
Causes
Perthes disease occurs when too little blood reaches the ball portion of the hip joint for a short time. Without enough blood, this bone becomes weak and collapses. The cause of the reduced blood flow is unknown.
Risk factors
Risk factors for Perthes disease include:
- Age. Perthes disease can affect children of nearly any age, but it most commonly begins between ages 4 and 10.
- Your child's sex. Perthes is about four times more common in boys than in girls.
Complications
Children who have had Perthes disease are at higher risk of developing hip arthritis in adulthood — especially if the hip joint has poor healing. If the ball-and-socket joint doesn't fit together well after healing, the joint can wear out early.
In general, children who are diagnosed with Perthes disease after age 6 are more likely to develop hip conditions later in life. The younger the child is at the time of diagnosis, the better the chances for the hip joint to heal in a typical, round shape.
Diagnosis
During the physical exam, your healthcare professional might move your child's legs into various positions to check range of motion and see whether any of the positions cause pain.
Imaging tests
These types of tests, which are vital to the diagnosis of Perthes disease, might include:
- X-rays. Initial X-rays may not show changes in the hip. It can take 1 to 2 months after symptoms begin for the changes related to Perthes disease to become clear on X-rays. Your healthcare professional will likely recommend several X-rays over time to track the progression of the disease.
- MRI. This technology uses radio waves and a strong magnetic field to make very detailed images of bone and soft tissue inside the body. MRIs often can visualize bone damage caused by Perthes disease more clearly than X-rays can, but MRI isn't always needed.
Treatment
In Perthes disease, the complete healing process can take several years. The types of treatment recommended depend on the:
- Age when symptoms began.
- Stage of the disease.
- Amount of hip damage.
As Perthes disease gets worse, the ball part of the joint, called the femoral head, weakens and breaks apart. During healing, the socket part of the joint can serve as a mold. This can help the weakened femoral head keep its round shape.
For this molding to work, the femoral head must sit snugly within the socket. Sometimes a child wears a special type of leg cast that spreads the legs widely apart for 4 to 6 weeks to keep the bone in the right position.
Some children need surgery to help keep the ball of the joint snug within the socket. This procedure might involve making wedge-shaped cuts in the thighbone or pelvis to align the joint again.
Surgery generally isn't needed for children younger than 6. In this age group, the hip socket is naturally more moldable, so the ball and socket usually continue to fit together well without surgery.
Other treatments
Some children, especially very young ones, might need only conservative treatments or observation. Conservative treatments can include:
- Activity restrictions. Children with Perthes disease should not run, jump or take part in other high-impact activities that might speed up hip damage.
- Crutches. Sometimes, your child may need to avoid bearing weight on the affected hip. Using crutches can help protect the joint.
- Physical therapy. As the hip stiffens, the muscles and ligaments around it may shorten. Stretching exercises can help keep the hip more flexible.
- Anti-inflammatory medicines. Your healthcare professional might recommend infants' or children's medicines that you can buy without a prescription, such as ibuprofen (Advil, Motrin, others) to help relieve your child's pain.
Preparing for an appointment
You'll probably first talk with your child's primary care team about your concerns. After an initial evaluation, your child might be referred to a doctor who specializes in bone conditions in children, called a pediatric orthopedic surgeon.
What you can do
Before your appointment, you may want to write a list of answers to the following questions:
- When did these symptoms begin?
- Does a particular leg position or activity make the pain worse?
- Did any of your blood relatives, such as a parent, aunt or grandparent, have similar symptoms when they were children?
- Does your child have any other medical problems?
- What medicines or supplements does your child take regularly?
What to expect from your doctor
Your healthcare team might ask some of the following questions:
- What are your child's symptoms?
- Have they gotten worse over time?
- Do the symptoms seem to come and go?
- Is your child active?
- Has your child had an accident or injury that might have caused hip damage?
- If your child's symptoms include pain, where is the pain located?
- Does activity make your child's symptoms worse?
- Does resting ease your child's discomfort?
© 1998-2026 Mayo Foundation for Medical Education and Research(MFMER). All rights reserved. Terms of Use
