Liver hemangioma
Conditions
Overview

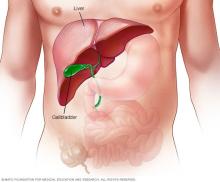
A liver hemangioma (he-man-jee-O-muh) is a noncancerous mass in the liver made up of a tangle of blood vessels. Liver hemangiomas are sometimes called hepatic hemangiomas or cavernous hemangiomas.
Most liver hemangiomas are found during a test done for another condition. These liver masses are common. Around 20% of the population is thought to have them. People who have a liver hemangioma rarely have symptoms and typically don't need treatment.
It may worry you to know that you have a mass in your liver, even if it's not cancerous. However, there's no evidence that an untreated liver hemangioma can lead to liver cancer.
Symptoms
In most cases, a liver hemangioma doesn't cause any symptoms. When it does cause symptoms, they may include:
- Pain in the upper right belly area.
- Feeling full after eating only a small amount of food.
- Nausea.
- Vomiting.
However, these symptoms are typically due to something else.
When to see a doctor
Make an appointment with your healthcare team if you have any ongoing symptoms that worry you.
Causes
It's not clear what causes a liver hemangioma to form. Healthcare professionals believe that liver hemangiomas are present at birth, also known as congenital.
A liver hemangioma usually grows as a single collection of tangled blood vessels and is typically less than about 1.5 inches (about 4 centimeters) wide. Sometimes liver hemangiomas can be larger or happen in multiples. Large hemangiomas can grow in young children, but this is rare.
In most people, liver hemangiomas do not grow or cause any symptoms. But in a small number of people, liver hemangiomas grow to cause symptoms and require treatment. It's not clear why this happens.
Risk factors
Factors that can increase the risk of a liver hemangioma include:
- Age. A liver hemangioma can be diagnosed at any age, but it's most often diagnosed in people ages 30 to 50.
- Being female. Women are more likely to be diagnosed with a liver hemangioma than are men.
- Pregnancy. Women who have been pregnant are more likely to develop a liver hemangioma than are women who have never been pregnant. It's believed the hormone estrogen, which rises during pregnancy, may play a role in liver hemangioma growth.
- Hormone replacement therapy. Women who use hormone replacement therapy for menopausal symptoms may be more likely to develop a liver hemangioma than are women who do not.
Complications
Women who have been diagnosed with liver hemangiomas have a higher risk of complications if they become pregnant. The hormone estrogen, which increases during pregnancy, is believed to cause some liver hemangiomas to grow larger.
Very rarely, a growing hemangioma can cause symptoms that may require treatment. Symptoms may include pain in the upper right corner of the belly area, stomach bloating or nausea. Having a liver hemangioma doesn't mean you can't become pregnant. However, talking about the possible complications with your healthcare team can help you make a more informed choice.
Diagnosis
Tests used to diagnose liver hemangiomas include:
- Ultrasound, an imaging method that uses sound waves to produce images of the liver.
- CT scan, which combines a series of X-ray images taken from different angles around the body and uses computer processing to create images of the liver.
- MRI scan, a technique that uses a magnetic field and radio waves to create detailed images of the liver.
Other tests may be used depending on your situation.
Treatment
If your liver hemangioma is small and doesn't cause any symptoms, you likely won't need treatment. In most people, liver hemangiomas do not grow or cause symptoms. You may be scheduled for occasional follow-up exams to see if your liver hemangioma is growing.
Liver hemangioma treatment depends on the location and size of the hemangioma, whether you have more than one hemangioma, your overall health, and your preferences.
Treatment options may include:
- Surgery to remove the liver hemangioma. If the hemangioma can be easily separated from the liver, surgery may be recommended to remove the mass.
- Surgery to remove part of the liver, including the hemangioma. In some people, surgeons may need to remove a part of the liver along with the hemangioma.
- Procedures to stop blood flow to the hemangioma. Without a blood supply, the hemangioma may stop growing or shrink. The blood flow may be stopped by tying off the main artery, a procedure called hepatic artery ligation. It also can be stopped by injecting medicine into the artery to block it. This procedure is known as arterial embolization. In both procedures, healthy liver tissue is not harmed because it can draw blood from other nearby vessels.
- Liver transplant surgery. In the rare event that you have a large hemangioma or multiple hemangiomas that can't be treated any other way, your healthcare professional may recommend a liver transplant.
- Radiation therapy. Radiation therapy uses powerful energy beams, such as X-rays, to damage the cells of the hemangioma. This treatment is rarely used because there are safer and more effective treatments.
Preparing for your appointment
Most liver hemangiomas are discovered during a test or procedure for something else. If your care team thinks you have a liver mass, you may be referred to a doctor who specializes in the digestive system, called a gastroenterologist, or one who specializes in the liver, called a hepatologist.
Here's some information to help you get ready for your appointment.
What you can do
- Be aware of anything you need to do ahead of time. At the time you make the appointment, ask if there's anything you need to do in advance, such as restrict your diet.
- Write down symptoms you have, including any that may not seem related to the reason you scheduled the appointment.
- Write down important personal information, including major stresses or recent life changes.
- Make a list of all medicines, vitamins and supplements you're taking and the doses.
- Take a family member or friend along. Sometimes it can be hard to remember all the information provided during an appointment. Someone who goes with you may remember something that you missed or forgot.
- Write down questions to ask your healthcare team.
Your time with your healthcare team is limited, so preparing a list of questions can help you make the most of your time together. List your questions from most important to least important in case time runs out. For liver hemangioma, some basic questions to ask include:
- What is the size of my liver hemangioma?
- Do I have one liver hemangioma or multiple hemangiomas?
- Is my liver hemangioma growing?
- What other tests do I need?
- Do I need treatment for my liver hemangioma?
- Are there brochures or other printed material that I can take with me? What websites do you recommend?
- Should I plan for a follow-up visit?
- Are there medicines that may worsen my hemangioma?
- Are my symptoms from the hemangioma?
Don't hesitate to ask other questions.
What to expect from your doctor
Be prepared to answer questions, such as:
- Have you had pain, nausea, loss of appetite or feelings of fullness after eating little?
- Have you been pregnant?
- Have you used hormone replacement therapy?
© 1998-2026 Mayo Foundation for Medical Education and Research(MFMER). All rights reserved. Terms of Use
