Mitral valve regurgitation
Conditions
Overview
Mitral valve regurgitation is the most common type of heart valve disease. In this condition, the valve between the left heart chambers doesn't close fully. Blood leaks backward across the valve. If the leakage is severe, not enough blood moves through the heart or to the rest of the body. Mitral valve regurgitation can make you feel very tired or short of breath.
Other names for mitral valve regurgitation are:
- Mitral regurgitation (MR).
- Mitral insufficiency.
- Mitral incompetence.
Treatment of mitral valve regurgitation may include regular health checkups, medicines or surgery. You may not need treatment if the condition is mild.
Severe mitral valve regurgitation often requires a catheter procedure or heart surgery to repair or replace the mitral valve. Without proper treatment, severe mitral valve regurgitation can cause heart rhythm problems or heart failure.
Symptoms
Mitral valve regurgitation is often mild and develops slowly. Some people do not have symptoms for many years.
But sometimes, mitral valve regurgitation develops quickly. When this happens, it's called acute mitral valve regurgitation.
Fatigue is a common but nonspecific symptom of mitral valve regurgitation. Other symptoms of mitral valve regurgitation include:
- Irregular heartbeat, called an arrhythmia.
- Shortness of breath, especially when lying down.
- Feelings of a rapid, pounding or fluttering heartbeat, called palpitations.
- Swollen feet or ankles.
When to see a doctor
If you have symptoms of mitral valve regurgitation, make an appointment for a health checkup.
You may be referred to a doctor trained in heart diseases, called a cardiologist.
Causes
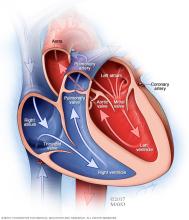
To understand the causes of mitral valve disease, it may be helpful to know how the heart works.
The mitral valve is one of four valves in the heart that keep blood flowing in the right direction. Each valve has flaps, also called leaflets, that open and close once during each heartbeat.
In mitral valve regurgitation, the valve flaps don't close tightly. Blood moves backward when the valve is closed. This makes it harder for the heart to work properly.
If mitral valve regurgitation is due to problems with the mitral valve, the condition is called primary mitral valve regurgitation.
If a problem or disease affecting other areas of the heart cause a leaky mitral valve, the condition is called functional or secondary mitral regurgitation.
Possible causes of mitral valve regurgitation include:
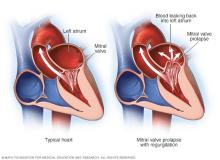
- Mitral valve prolapse. In this condition, the mitral valve's flaps bulge back into the left upper heart chamber when the heart squeezes. This common heart problem can prevent the mitral valve from closing tightly and cause blood to flow backward.
- Rheumatic fever. Rheumatic fever is a complication of untreated strep throat. Rheumatic fever can damage the mitral valve, leading to mitral valve regurgitation early or later in life. If rheumatic fever causes mitral valve disease, the condition is called rheumatic mitral valve disease. Rheumatic fever is rare in the United States.
- Heart attack. A heart attack can damage the area of the heart muscle that supports the mitral valve. If there is a lot of heart attack damage, sudden and severe mitral valve regurgitation can occur. A leaky mitral valve caused by a heart attack is called ischemic mitral regurgitation.
- Heart problem present at birth, also called a congenital heart defect. Some people are born with heart structure problems, including damaged heart valves.
- Thickening of the heart muscle, called cardiomyopathy. Cardiomyopathy makes it harder for the heart to pump blood to the rest of the body. The condition can affect how the mitral valve works, causing regurgitation. Types of cardiomyopathy linked to mitral valve regurgitation include dilated cardiomyopathy and hypertrophic cardiomyopathy.
- Damaged tissue cords. Over time, the pieces of tissue that hold the flaps of the mitral valve to the heart wall may stretch or tear. This is especially likely in people with mitral valve prolapse. A tear can cause blood to suddenly leak through the mitral valve. It may require mitral valve repair surgery. A chest injury also can cause rupture of the cords.
- Inflammation of the inner lining of the heart's chambers and valves, called endocarditis. This condition is usually caused by an infection. Germs get into the bloodstream and attach to damaged areas in the heart.
- Radiation therapy. Rarely, radiation therapy for cancer that is focused on the chest area can lead to mitral valve regurgitation.
Risk factors
Several things can increase the risk of mitral valve regurgitation, including:
- Certain infections that affect the heart.
- Heart attack.
- Heart problems present at birth, called congenital heart defects.
- History of other heart valve diseases, including mitral valve prolapse and mitral valve stenosis.
- Older age.
- Radiation to the chest.
Complications
Mitral valve regurgitation complications often depend on the severity of disease. Mild mitral valve regurgitation usually does not cause any problems.
As mitral valve regurgitation gets worse, the heart must work harder to pump blood to the body. The strain on the heart can cause the left lower chamber to widen. The heart muscle may become weak.
Potential complications of severe mitral valve regurgitation include:
- An irregular and often rapid heartbeat, called atrial fibrillation. Mitral valve regurgitation may trigger this common heart rhythm disorder. Atrial fibrillation has been linked to an increased risk of blood clots and stroke.
- High blood pressure in the lungs, called pulmonary hypertension. Long-term untreated or improperly treated mitral regurgitation can increase pressure in the blood vessels in the lungs. As pressure rises, fluid builds up in the lungs.
- Congestive heart failure. In severe mitral valve regurgitation, the heart has to work harder to pump enough blood to the body. The extra effort causes the left lower heart chamber to get bigger. Untreated, the heart muscle becomes weak. This can cause heart failure.
Diagnosis
To diagnose mitral valve regurgitation, a health care professional does a physical exam and asks questions about your symptoms and medical history. A device called a stethoscope is used to listen to the heart and lungs. If you have mitral valve regurgitation, a whooshing sound called a murmur may be heard. The mitral valve heart murmur is the sound of blood leaking backward through the valve.
Tests may be done to confirm a diagnosis of mitral valve regurgitation or to check for other conditions that can cause similar symptoms.
Tests
Common tests to diagnose mitral valve regurgitation include:
-
Echocardiogram. Sound waves are used to create pictures of the beating heart. An echocardiogram shows the structure of the mitral valve and blood flow in the heart. A standard echocardiogram is called a transthoracic echocardiogram (TTE). It can confirm a diagnosis of mitral valve regurgitation. The test also can tell how severe the condition is. Echocardiography also can help diagnose congenital mitral valve disease, rheumatic mitral valve disease and other heart valve conditions.
Sometimes, a more-detailed echocardiogram is needed to better see the mitral valve. This test is called a transesophageal echocardiogram (TEE). A TEE creates pictures of the heart from inside the body.
- Electrocardiogram (ECG). This test shows how the heart is beating. Sticky patches called sensors are attached to the chest and sometimes the arms and legs. Wires connect the patches to a computer, which displays or prints results. An ECG can show irregular heart rhythms related to mitral valve disease.
- Chest X-ray. A chest X-ray shows the condition of the heart and lungs. This quick test can help diagnose an enlarged heart or fluid in the lungs.
- Cardiac MRI. This test uses magnetic fields and radio waves to create detailed pictures of the heart. Cardiac MRI may help show the severity of mitral valve regurgitation. The test also gives details about the lower left heart chamber.
- Exercise tests or stress tests. These tests often involve walking on a treadmill or riding a stationary bike while the heart is checked. Exercise tests show how the heart reacts to physical activity. The tests can show whether mitral valve regurgitation symptoms occur during exercise. If you can't exercise, you might be given medicine that makes the heart work like exercise does.
- Cardiac catheterization.This test isn't often used to diagnose mitral valve disease. But it can be helpful if other tests haven't diagnosed the condition. A doctor guides a thin, flexible tube called a catheter through a blood vessel in the arm or groin. It's moved to an artery in the heart. Dye flows through the tube. This makes the arteries in the heart chambers show up more clearly on X-rays taken during the test.
Staging
After testing confirms a diagnosis of mitral or other heart valve disease, your health care team may tell you the stage of disease. Staging helps determine the most appropriate treatment.
The stage of heart valve disease depends on many things, including symptoms, disease severity, the structure of the valve or valves, and blood flow through the heart and lungs.
Heart valve disease is staged into four basic groups:
- Stage A: At risk. Risk factors for heart valve disease are present.
- Stage B: Progressive. Valve disease is mild or moderate. There are no heart valve symptoms.
- Stage C: Asymptomatic severe. There are no heart valve symptoms, but the valve disease is severe.
- Stage D: Symptomatic severe. Heart valve disease is severe and is causing symptoms.
Outlook
How well a person does after being diagnosed with mitral valve regurgitation varies. This is called the outlook, also called prognosis. The outlook for mitral valve regurgitation depends on:
- The cause of the mitral valve disease.
- The stage of heart valve disease.
- The severity of regurgitation.
- How long the condition has been present, also called the duration.
Treatment


The goals of mitral valve regurgitation treatment are to:
- Help the heart work better.
- Reduce symptoms.
- Prevent complications.
Some people, especially those with mild regurgitation, might not need treatment. Your health care team considers your symptoms and stage of regurgitation, among other things, when planning treatment.
Treatment of mitral valve regurgitation may include:
- Healthy lifestyle changes.
- Regular health checkups.
- Medicines to treat symptoms and prevent complications, such as blood clots.
- Surgery to repair or replace the mitral valve.
A doctor trained in heart diseases typically provides care for people with mitral valve regurgitation. This type of health care professional is called a cardiologist.
If you have mitral valve regurgitation, consider being treated at a medical center with a multidisciplinary team of health care professionals trained and experienced in evaluating and treating heart valve disease.
Medications
Medicines may be needed to reduce mitral valve regurgitation symptoms and to prevent complications of heart valve disease.
Types of medicines that may be used for mitral valve regurgitation include:
- Water pills, also called diuretics. This medicine reduces or prevents fluid buildup in the lungs and other parts of the body.
- Blood thinners, also called anticoagulants. If you have atrial fibrillation due to mitral valve disease, such as mitral valve regurgitation, your health care team may recommend these medicines to prevent blood clots. Atrial fibrillation increases the risk of blood clots and stroke.
- Blood pressure medicines. High blood pressure makes mitral valve regurgitation worse. If you have mitral valve regurgitation and high blood pressure, you may be given medicines to lower blood pressure.
Surgery or other procedures
A diseased or damaged mitral valve might eventually need to be repaired or replaced, even if you don't have symptoms. Surgery for mitral valve disease includes mitral valve repair and mitral valve replacement. Your health care team discusses the risks and benefits of each type of heart valve with you to determine which valve may be best for you.
If you need surgery for another heart condition, a surgeon might perform mitral valve repair or replacement at the same time as that other surgery.
Mitral valve surgery is usually done through a cut in the chest. Surgeons at some medical centers sometimes use robot-assisted heart surgery, a minimally invasive procedure in which robotic arms are used to do the surgery.
Mitral valve repair
Mitral valve repair saves the existing valve and may save heart function. Whenever possible, mitral valve repair is recommended before considering valve replacement. People who have mitral valve repair for mitral regurgitation at an experienced medical center generally have good outcomes.
During mitral valve repair surgery, the surgeon might:
- Patch holes in a heart valve.
- Reconnect the valve flaps.
- Remove excess tissue from the valve so that the flaps can close tightly.
- Repair the structure of the mitral valve by replacing cords that support it.
- Separate valve leaflets that have connected.
Other mitral valve repair procedures include:
- Annuloplasty. A surgeon tightens or reinforces the ring around the valve, called the annulus. Annuloplasty may be done with other techniques to repair a heart valve.
- Valvuloplasty. This treatment is used to repair a mitral valve with a narrowed opening. It might be done even if you don't have symptoms. It's done using a thin tube called a catheter with a balloon on the tip. The surgeon inserts the tube into an artery in the arm or groin and guides it to the mitral valve. The balloon is inflated, widening the mitral valve opening. The balloon is then deflated, and the catheter and balloon are removed.
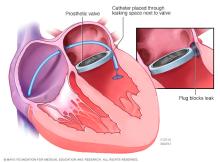
- Mitral valve clip. In this treatment, a doctor guides a catheter with a clip on its end to the mitral valve through an artery in the groin. The clip is used to improve the closure of the mitral valve leaflets. It reduces the amount of regurgitation. This procedure is an option for people who have severe mitral valve regurgitation or who aren't good candidates for mitral valve surgery.
Mitral valve replacement
During mitral valve replacement, the surgeon removes the mitral valve. It's replaced with a mechanical valve or a valve made from cow, pig or human heart tissue. A tissue valve also is called a biological tissue valve.
Sometimes, a heart catheter procedure is done to put a replacement valve into a biological tissue valve that no longer works well. This is called a valve-in-valve procedure.
If you had mitral valve replacement with a mechanical valve, you need to take blood thinners for life to prevent blood clots. Biological tissue valves break down over time and usually need to be replaced.
Lifestyle and home remedies
Your health care team may suggest that you make several heart-healthy lifestyle changes. Take these steps:
- Manage blood pressure. Control of high blood pressure is important if you have mitral valve regurgitation.
- Eat a heart-healthy diet. Food doesn't directly affect mitral valve regurgitation. But a healthy diet can help prevent other heart disease that can weaken the heart muscle. Eat foods that are low in saturated and trans fats, sugar, salt, and refined grains, such as white bread. Eat a variety of vegetables and fruits, whole grains, and proteins, such as lean meats, fish and nuts.
- Get regular exercise. How long and hard you're able to exercise can depend on whether you have mild, moderate or severe mitral valve regurgitation. Talk with your health care team about the amount and type of exercise that's best for you, especially if you're considering competitive sports.
- Maintain a healthy weight. Being overweight increases the risk of heart disease. Talk with a health care professional to set realistic goals for body mass index and weight.
- Prevent infective endocarditis. If you've had mitral valve replacement, your doctor will likely recommend that you take antibiotics before dental procedures to prevent an infection called infective endocarditis.
- Avoid or limit alcohol. Heavy alcohol use can cause irregular heartbeats and can make your symptoms worse. Excessive alcohol use also can cause a weakened heart muscle that leads to mitral regurgitation. Ask your health care team about the effects of drinking alcohol.
- Avoid tobacco. If you smoke, quit. Ask your health care team about resources to help you quit smoking. Joining a support group may be helpful.
- Practice good sleep habits. Poor sleep may increase the risk of heart disease and other chronic conditions. Go to bed and wake at the same time every day, including on weekends. If you have trouble sleeping, talk with a health care professional about strategies that might help.
If you have mitral valve regurgitation and are thinking about getting pregnant, talk with your health care team first. Pregnancy causes the heart to work harder. How a heart with mitral valve regurgitation tolerates this extra work depends on the degree of regurgitation and how well the heart pumps.
Preparing for an appointment
If you think you have mitral valve regurgitation, make an appointment to see a health care professional. Here's some information to help you prepare for your appointment.
What you can do
- Be aware of pre-appointment restrictions. When you make the appointment, ask if there's anything you need to do beforehand.
- Write down your symptoms, including any that seem unrelated to mitral valve regurgitation.
- Write down important personal information, including a family history of heart disease, heart problems present from birth, genetic conditions, stroke, high blood pressure or diabetes, and any major stresses or recent life changes.
- Make a list of all medications, vitamins and supplements you take. Include the dosages.
- Take a family member or friend along, if possible, to help you remember information you receive.
- Be prepared to discuss your diet and exercise habits. . If you don't already eat well and exercise, be ready to talk with your health care team about challenges you might face in getting started.
- Write down questions to ask your health care team.
For mitral valve regurgitation, some basic questions to ask a health care professional include:
- What is likely causing my condition?
- What are other possible causes for my symptoms?
- What tests will I need?
- What's the best treatment?
- What are other treatment options?
- I have other health conditions. How can I best manage them together?
- Are there restrictions I need to follow?
- If I need surgery, which surgeon do you recommend for mitral valve repair?
- Are there brochures or other printed material I can take with me? What websites do you recommend?
Don't hesitate to ask other questions you have.
What to expect from your doctor
Your health care team is likely to ask you many questions, including:
- When did your symptoms begin?
- Are your symptoms constant or do they come and go?
- How severe are your symptoms?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
© 1998-2026 Mayo Foundation for Medical Education and Research(MFMER). All rights reserved. Terms of Use
