Pelvic inflammatory disease (PID)
Conditions
Overview

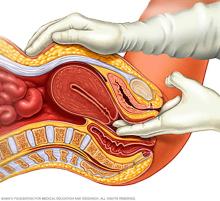
Pelvic inflammatory disease, also called PID, is an infection of the reproductive organs of people assigned female at birth. It most often happens when sexually transmitted germs spread from the vagina to the uterus, fallopian tubes or ovaries.
The symptoms of pelvic inflammatory disease may be mild. Some people have no symptoms. If you don't have symptoms, you might not realize you have pelvic inflammatory disease until you have trouble getting pregnant or you get ongoing, called chronic, pelvic pain.
Symptoms
The symptoms of pelvic inflammatory disease might be mild. Some people don't have symptoms. Symptoms may include:
- Pain in the lower belly and pelvis.
- Fluid that comes out of the vagina, called discharge, that's heavy or not usual. It may smell bad.
- Bleeding from the vagina between periods.
- Pain during sex.
- Fever, sometimes with chills.
- Urinating often. It may cause a burning feeling.
When to see a doctor
See your healthcare professional right away or seek emergency care if you have:
- Strong pain.
- Upset stomach and vomiting.
- A temperature higher than 101 degrees Fahrenheit (38.3 degrees Celsius).
Even if your PID symptoms don't bother you much, see your healthcare professional as soon as you can. Vaginal discharge with an odor, painful urination or bleeding between periods can be symptoms of a sexually transmitted infection, also called an STI.
If you have these symptoms, don't have sex. And make an appointment with your healthcare professional. Fast treatment of an STI can help prevent PID.
Causes
Many types of germs can cause PID. But gonorrhea and chlamydia are the most common. You may get these germs during sex if you don't use protection, such as a condom.
Other germs also can cause pelvic inflammatory disease. These include bacteria in the vagina that are typical but out of balance. This is called bacterial vaginosis.
Rarely, germs may enter the reproductive tract when a healthcare professional puts in an intrauterine device, also called an IUD, for long-term birth control. Any medical procedure that involves putting instruments into the uterus also can cause PID.
Risk factors
Factors that might increase your risk of pelvic inflammatory disease include:
- Being sexually active and younger than 25 years old.
- Having more than one sex partner.
- Having sex with someone who has more than one sex partner.
- Having sex without using a condom the right way.
- Douching. This upsets the balance between good germs and harmful ones in the vagina. Douching might mask symptoms of PID.
- Having had pelvic inflammatory disease or a sexually transmitted infection.
Complications
Pelvic inflammatory disease may cause scar tissue and pockets of infected fluid, called abscesses, in the reproductive tract. These can cause lasting damage to the reproductive organs.
Complications from this damage might include:
- Ectopic pregnancy. PID is a major cause of ectopic pregnancy, also called tubal pregnancy. An ectopic pregnancy can happen when PID causes scar tissue in one of the tubes that links the uterus to the ovaries, called the fallopian tubes. The scar tissue keeps the fertilized egg from making it through the fallopian tube to the uterus.
The fertilized egg then grows in the fallopian tube. Ectopic pregnancies can cause life-threatening bleeding and need emergency medical attention.
- Trouble getting pregnant. Damage to your reproductive organs can keep you from getting pregnant, called infertility. The more times you've had PID, the greater your risk of infertility. Delaying treatment for PID also greatly raises your risk of infertility.
- Ongoing, called chronic, pelvic pain. Pelvic inflammatory disease can cause pelvic pain that might last for months or years. Scarring in the fallopian tubes and other pelvic organs can cause pain during sex and when the body releases an egg, called ovulation.
- Tubo-ovarian abscess. PID might cause pus to form in the reproductive tract. This is called an abscess. Most often, abscesses affect the fallopian tubes and ovaries. But they can form in the uterus or in other pelvic organs. An abscess may turn into a life-threatening infection.
Prevention
To lower your risk of pelvic inflammatory disease:
- Practice safer sex. Use condoms every time you have sex, limit your number of partners and ask about a partner's sexual history before you have sex.
- Talk with your healthcare professional about birth control. Many forms of birth control don't protect against getting PID. Using barrier methods, such as a condom, helps lower the risk. Even if you take birth control pills, use a condom every time you have sex with a new partner to protect against STIs.
- Get tested. If you're at risk of an STI, make an appointment with your healthcare professional for testing. Set up a regular screening schedule with your healthcare professional if needed. Early treatment of an STI gives you the best chance of not getting PID.
- Ask your partner to be tested. If you have pelvic inflammatory disease or an STI, ask your partner to be tested and treated. This can prevent the spread of STIs and keep PID from coming back.
- Don't douche. Douching upsets the balance of germs in the vagina.
Diagnosis
No single test can diagnose pelvic inflammatory disease. (3p2) Instead, your healthcare professional will rely on:
- Your medical history. This includes your sexual habits, sexually transmitted infections you've had and the birth control you use.
- Your symptoms. Tell your healthcare professional about any symptoms you have, even if they're mild.
- A pelvic exam. During the exam, your healthcare professional checks your pelvic area for tenderness and swelling. Your healthcare professional also may use cotton swabs to take fluid samples from your vagina and cervix. A lab tests the samples for signs of infection.
- Blood and urine tests. These can test for pregnancy, HIV and other sexually transmitted infections. They also can measure white blood cell counts or other markers of infection.
- Ultrasound. This test uses sound waves to make images of the reproductive organs.
If the diagnosis still isn't clear, you may need other tests, such as:
- Laparoscopy. During this procedure, a healthcare professional puts a thin, lighted tube through a small cut, called an incision, in the belly to view the pelvic organs.
- Endometrial biopsy. During this procedure, a healthcare professional puts a thin tube into the uterus to remove a small sample of its lining, called endometrial tissue. A lab tests the tissue for signs of infection.
Treatment
Fast treatment with medicine can get rid of the infection that causes pelvic inflammatory disease. But there's no way to fix scarring or other damage to the reproductive tract that PID can cause. Treatment for PID most often includes:
- Antibiotics. Your healthcare professional prescribes a mix of antibiotics to start right away. After getting your lab test results, your healthcare professional might change your prescription to better match what's causing the infection.
Follow up with your healthcare professional after three days to make sure the treatment is working. Be sure to take all your medicine, even if you start to feel better after a few days.
- Treatment for your partner. To prevent getting infected again with an STI, your sexual partner or partners should be checked and treated. Infected partners might not notice any symptoms.
- No sex. Don't have sexual intercourse until you complete treatment and your symptoms have cleared.
If you are pregnant, are very ill, might have an abscess or haven't responded to medicines that you take by mouth, you may need to go to a hospital. You may get antibiotics through a vein in your arm, called intravenous. Then you get antibiotics to take by mouth.
Surgery is rarely needed. But if an abscess bursts or threatens to burst, your healthcare professional might drain it. You also may need surgery if you don't respond to antibiotic treatment.
Coping and support
Pelvic inflammatory disease can cause distress. You may be dealing with the diagnosis of a sexually transmitted infection. You may have ongoing pain or find that you can't have children. Try these tips to help you cope with your diagnosis:
- Get treatment. A sexually transmitted infection most often causes PID. Having an STI may upset you, but you and your partner should both get treatment right away. Treatment can keep PID from getting worse and prevent getting the infection again.
- Be aware of infertility. If you've had pelvic inflammatory disease more than once, you're at greater risk of not being able to have children. If you've been trying to get pregnant without success, make an appointment to have your fertility checked. Ask your healthcare professional about infertility testing and treatment. Knowing about the process may help ease your concerns.
- Seek support. Sexual health, infertility and chronic pain may be very personal. But reach out to your partner, close family members or friends, or a healthcare professional for support. Many online support groups let you talk about your concerns without saying who you are.
Preparing for your appointment
If you have symptoms of pelvic inflammatory disease, make an appointment to see your healthcare professional.
Here's some information to help you get ready for your appointment
What you can do
Make a list of:
- Any symptoms you have, and when they began.
- All medicines, vitamins and supplements you take, including dosages.
- Questions to ask during your appointment.
Some basic questions to ask include:
- What tests do I need?
- Is this a sexually transmitted infection?
- Should my partner be tested or treated?
- Do I need to stop having sex during treatment? How long should I wait?
- How can I keep from getting pelvic inflammatory disease again?
- Will this keep me from having children?
- Do you have printed materials that I can have? What websites do you suggest?
What to expect from your doctor
Be ready to answer questions, such as:
- Do you have a new sexual partner or more than one partner?
- Do you always use condoms?
- Do you have pelvic pain?
- How much do your symptoms bother you?
© 1998-2026 Mayo Foundation for Medical Education and Research(MFMER). All rights reserved. Terms of Use
