Polycythemia vera
Conditions
Overview
Polycythemia vera (pol-e-sy-THEE-me-uh VEER-uh) is a type of blood cancer. It causes the bone marrow to make too many red blood cells. These extra cells thicken the blood, slowing its flow. This may cause serious problems, such as blood clots.
Polycythemia vera is rare. It comes on slowly. You might have it for years without knowing. Often the condition is found during a blood test done for another reason.
Without treatment, polycythemia vera can be life-threatening. But proper medical care can help ease symptoms and complications of this disease.
Symptoms
Many people with polycythemia vera don't notice symptoms. Some people get symptoms such as headache, dizziness, tiredness and blurred vision.
Clearer symptoms of polycythemia vera include:
- Itchiness, mostly after a warm bath or shower.
- Numbness, tingling, burning or weakness in the hands, feet, arms or legs.
- A feeling of fullness soon after eating.
- Bloating or pain in the left upper stomach area due to an enlarged spleen.
- Unusual bleeding, such as a nosebleed or bleeding gums.
- Painful swelling of one joint, often the big toe.
- Shortness of breath and trouble breathing when lying down.
- Bone pain.
When to see a doctor
Make an appointment with your healthcare professional if you have symptoms of polycythemia vera.
Causes
Polycythemia vera happens when a change in a gene causes a problem with making blood cells. The body typically controls the number of each of the three types of blood cells. These are red blood cells, white blood cells and platelets. But in polycythemia vera, the bone marrow makes too many of some of these blood cells.
The cause of the gene change in polycythemia vera is unknown. But it's not passed through families.
Risk factors
Polycythemia vera can happen at any age. But it's more common in adults over age 60. Men are more likely to get polycythemia vera than women are.
Complications
Possible complications of polycythemia vera include:
- Blood clots. Increased blood thickness, decreased blood flow and atypical platelets raise the risk of blood clots. Blood clots can cause a stroke or a heart attack. Or clots can block an artery in the lungs or a vein deep within a leg muscle or in the belly.
- Enlarged spleen. The spleen helps the body fight infection. It also filters waste, such as old or damaged blood cells. The extra blood cells that occur with polycythemia vera make the spleen work harder. That causes it to enlarge.
- Problems due to high levels of red blood cells. Too many red blood cells can lead to other complications. These include open sores on the inside lining of the stomach, upper small intestine or esophagus, called peptic ulcers, and swelling of the joints, called gout.
- Other blood disorders. In rare cases, polycythemia vera can lead to other blood diseases. These include a disorder in which scar tissue replaces bone marrow, a condition in which stem cells don't mature or work as they should, and cancer of the blood and bone marrow, called acute leukemia.
Diagnosis
Your healthcare professional takes a medical history and do a physical exam.
Blood tests
If you have polycythemia vera, blood tests might show:
- More red blood cells than usual and, sometimes, an increase in platelets or white blood cells.
- A higher portion of red blood cells that make up total blood volume, called hematocrit measurement.
- Higher level of the iron-rich protein in red blood cells that carries oxygen, called hemoglobin.
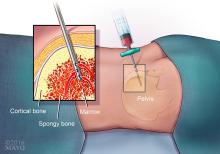
Bone marrow aspiration or biopsy
A healthcare professional who suspects that you have polycythemia vera might suggest getting a sample of your bone marrow through a bone marrow aspiration or biopsy.
A bone marrow biopsy involves taking a sample of the spongy tissue in bone marrow. A bone marrow aspiration often is done at the same time to get a sample of the liquid portion of your marrow.
Gene testing
Study of your bone marrow or blood might show the gene change that's linked with the disease.
Treatment
There's no cure for polycythemia vera. Treatment aims to lower your risk of complications. Treatments also might ease your symptoms.
Blood withdrawals
The most common treatment for polycythemia vera is having blood withdrawn often. This is done using a needle in a vein, called phlebotomy. It's the same procedure used for donating blood.
This lowers your blood volume and reduces the number of excess blood cells. How often you need to have blood withdrawn depends on how severe your condition is.
Treatments to reduce itching
If the condition causes itching, medicines such as antihistamines or treatments with ultraviolet light might give you relief.
Medicines that are used to treat depression, called selective serotonin reuptake inhibitors (SSRIs), helped relieve itching in clinical trials. SSRIs include paroxetine (Brisdelle, Paxil) or fluoxetine (Prozac, Symbyax).
Medicines that lower the number of red blood cells
If phlebotomy doesn't help enough, these medicines can lower the number of red blood cells in your blood:
- Hydroxyurea (Droxia, Hydrea, Siklos).
- Interferon alfa-2b (Intron A).
- Ruxolitinib (Jakafi).
- Busulfan (Busulfex, Myleran).
Heart medicines
Your healthcare professional also will likely prescribe medicines to control risk factors for heart and blood vessel disease. These include high blood pressure, diabetes and high cholesterol.
You also might take a low dose of aspirin to reduce your risk of blood clots. Low-dose aspirin also may help reduce burning pain in your feet or hands.
Self care
Here are ways to feel better if you have polycythemia vera:
- Exercise. Gentle exercise, such as walking, can improve blood flow. This helps lower the risk of blood clots. Leg and ankle stretches and exercises also can improve blood flow.
- Don't use tobacco. Using tobacco can narrow your blood vessels. This raises the risk of heart attack or stroke due to blood clots.
- Don't go places with low oxygen levels. Living at high altitudes, skiing or climbing in mountains all reduce the oxygen levels in your blood.
-
Be good to your skin. To reduce itching, bathe in cool water, use a gentle cleanser and pat your skin dry. Adding starch, such as cornstarch, to your bath might help. Don't use hot tubs or heated whirlpools. Don't take hot showers or baths.
Try not to scratch. Scratching can hurt your skin and raise the risk of infection. Use lotion on your skin to keep it moist.
-
Take care in hot and cold temperatures. Poor blood flow increases your risk of injury from hot and cold temperatures. In cold weather, always wear warm clothing. Keep your feet and hands warm.
In hot weather, protect yourself from the sun. Drink plenty of liquids.
- Watch for sores. Poor blood flow can make it hard for sores to heal. Look at your hands and feet often. Tell your healthcare professional about any sores.
Preparing for your appointment
You're likely to start by seeing your primary health professional. If you have with polycythemia vera, you might be sent to a specialist in blood conditions, called a hematologist.
Here's some information to help you get ready for your appointment.
What you can do
Make a list of:
- All your symptoms and when they began.
- Key personal information, including other medical conditions and family medical history.
- All medicines, vitamins or supplements you take, including doses and how often you take them.
- Questions to ask your healthcare professional.
For polycythemia vera, questions to ask include:
- What's the most likely cause of my symptoms?
- What tests do I need?
- Will this condition go away, or will I always have it?
- What treatments are available? Which do you suggest?
- I have other health conditions. How can I best manage them together?
- Should I see a specialist?
- Will I need follow-up visits? If so, how often?
- Are there brochures or other printed material I can have? What websites do you suggest?
Don't hesitate to ask other questions you have. Take a family member or friend along, if possible, to help you remember the information you're given.
What to expect from your doctor
Your healthcare professional is likely to ask you questions, including
- Do you have symptoms all the time, or do they come and go?
- How do your symptoms affect your life?
- What, if anything, seems to make your symptoms better?
- Does anything make your symptoms worse?
© 1998-2026 Mayo Foundation for Medical Education and Research(MFMER). All rights reserved. Terms of Use
