Reactive arthritis
Conditions
Overview
Reactive arthritis is a condition that causes joint pain and swelling, also called inflammation, after an infection in another part of the body. The infection typically starts in the gut, genitals or urinary tract.
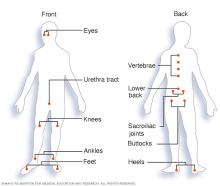
This condition typically affects the knees, ankles and feet. It also can cause inflammation in the eyes, the skin and the tube that carries urine out of the body, called the urethra. In the past, reactive arthritis was sometimes called Reiter syndrome.
Reactive arthritis is generally regarded as a form of spondyloarthritis (SpA). SpA is a group of inflammatory diseases that mainly affect the spine, joints, and places where tendons and ligaments attach to bones. The word comes from spondylo, meaning spine, and arthritis, meaning joint inflammation. SpA also is called enthesitis. These conditions share similar symptoms and genetic links, especially a gene called HLA-B27.
Reactive arthritis isn't common and typically happens for a limited time. For most people, symptoms come and go and usually disappear within a year.
Symptoms
The symptoms of reactive arthritis typically start 1 to 4 weeks after you've had a triggering infection. Common symptoms include:
- Pain and stiffness. This often affects the knees, ankles and feet. You may also feel pain in your heels, lower back or buttocks.
- Eye inflammation. Many people with reactive arthritis also develop red, irritated or painful eyes. These symptoms may be signs of conjunctivitis, commonly known as pink eye. Blurred vision also may be a symptom.
- Urinary issues. You may need to urinate more often. You may feel burning or discomfort when you do. In some people, there may be inflammation of the prostate gland or the cervix.
- Inflammation of tendons and ligaments where they attach to bone, called enthesitis. This happens most often in the heels and the soles of the feet.
- Swollen toes or fingers. They may become so swollen that they look like sausages.
- Skin issues. Some people get mouth sores, painless ulcers on the penis, or a rash on the palms of the hands or soles of the feet.
- Low back pain. The pain tends to be worse at night or in the morning.
When to see a doctor
If you develop joint pain within a month of having diarrhea or a genital infection, contact your healthcare professional.
Causes
Reactive arthritis happens when the immune system reacts to an infection somewhere else in the body — usually in the intestines, genitals or urinary tract. Sometimes the infection is so mild that you may not even know you had it.
Reactive arthritis itself is not contagious, but the bacteria that cause it can spread through sex or food. Several types of bacteria can trigger reactive arthritis. Common examples include:
- Chlamydia trachomatis. It is spread through sexual contact. The infection typically starts in the urethra, bladder or vagina.
- Clostridium difficile (C. difficile), Escherichia coli (E. coli), campylobacter, salmonella, shigella and yersinia. These bacteria typically infect the gastrointestinal tract, causing diarrhea or other stomach and intestinal symptoms.
Only a small number of people who are exposed to these bacteria develop reactive arthritis.
Risk factors
Certain factors increase the risk of reactive arthritis:
- Age. It most often affects adults between 20 and 40 years old.
- Sex assigned at birth. People are equally likely to get reactive arthritis from foodborne infections. But people assigned male at birth are more likely to develop it after a sexually transmitted infection.
- Genetics. Having a certain genetic marker (HLA-B27) increases the risk. But most people with this marker never get reactive arthritis.
- Infection. Having HIV increases the risk of developing reactive arthritis.
Prevention
You can't change your genes, but you can lower your risk of reactive arthritis by reducing exposure to bacteria that cause infections.
- Practice food safety. Keep food at the right temperature and cook it thoroughly to avoid bacteria that can cause reactive arthritis.
- Prevent sexually transmitted infections. Use condoms to help protect you from bacteria such as chlamydia that may trigger reactive arthritis.
Diagnosis
To diagnose reactive arthritis, your healthcare professional starts with a physical exam. They check your joints for swelling, warmth and tenderness. You may have tests to look at how well you can move your spine and affected joints. Your healthcare professional also may look at your eyes for signs of inflammation and examine your skin for rashes.
Blood tests
A blood test can help look for signs that support the diagnosis. Your healthcare professional may check for:
- A current or past infection.
- Inflammation in your body.
- Antibodies that could point to other types of arthritis.
- A genetic marker called HLA-B27 that is sometimes linked to reactive arthritis.
Joint fluid tests
Your healthcare professional may take a small sample of fluid from an affected joint using a needle. This test helps rule out other conditions. The fluid is tested for:
- White blood cells. High levels can mean inflammation or infection.
- Bacteria. The presence of bacteria may mean a joint infection called septic arthritis. This type of infection can cause serious joint damage.
- Crystals. Uric acid crystals may indicate gout, another type of painful arthritis that often affects the big toe.
Imaging tests
X-rays of your low back, pelvis and joints can help show typical signs of reactive arthritis or rule out other forms of arthritis.
Treatment
The main goals of treatment are to relieve your symptoms and treat any infection that may still be present. Because reactive arthritis may affect different parts of the body, more than one doctor or other healthcare professional may be involved in your care.
Medicines
If your reactive arthritis was caused by a bacterial infection, your healthcare professional may prescribe an antibiotic to treat it. Which antibiotic you take depends on the type of bacteria found.
Symptoms of reactive arthritis may be eased with:
- Nonsteroidal anti-inflammatory drugs (NSAIDs). Prescription NSAIDs, such as indomethacin (Indocin), can relieve the inflammation and pain of reactive arthritis.
- Steroids. A steroid injection into a painful joint can lessen inflammation and help you move more comfortably. Steroid eye drops may help with eye symptoms. Steroid creams can be used for skin rashes. And you may take steroids in pill form.
- Rheumatoid arthritis medicines. For ongoing pain and stiffness, medicines such as sulfasalazine (Azulfidine), methotrexate (Trexall) or etanercept (Enbrel) may be helpful for some people. Etanercept typically is used to treat rheumatoid arthritis.
Physical therapy
A physical therapist can teach you exercises to strengthen the muscles around affected joints and improve flexibility.
- Strengthening exercises support the joints and reduce strain.
- Range-of-motion exercises help you stay flexible and prevent stiffness.
Preparing for your appointment
You'll likely start by seeing your primary healthcare professional. They may refer you to a doctor who specializes in arthritis, called a rheumatologist, for further testing or treatment.
What you can do
When you make the appointment, ask if there's anything you need to do in advance, such as fasting before having a specific test.
Make a list of:
- Your symptoms, even ones that don't seem related to the reason you made the appointment.
- Your medical and family history.
- All medicines, vitamins or supplements you take, including doses.
- Questions you want to ask.
Take a family member or friend along, if possible. They can help you remember information and ask questions. Good questions to ask include:
- What is likely causing my symptoms or condition?
- What are other possible causes?
- What tests do I need?
- What treatment approach do you recommend?
- When should I expect to feel better?
- Is there anything I can do to lessen my joint pain now?
- Am I at risk of long-term complications?
- How can I manage this along with my other health conditions?
Don't hesitate to ask about anything else that concerns you.
What to expect from your doctor
Your healthcare professional may ask you questions such as:
- When did your symptoms start?
- Do they come and go, or do they happen all the time?
- How serious is your pain or stiffness?
- What makes your symptoms better or worse?
- Have you had any recent infections?
© 1998-2026 Mayo Foundation for Medical Education and Research(MFMER). All rights reserved. Terms of Use
