Solitary rectal ulcer syndrome
Conditions
Overview
Solitary rectal ulcer syndrome is a condition in which one or more open sores, called ulcers, form in the rectum. The rectum is a muscular tube connected to the end of the colon. Stool passes through the rectum on its way out of the body.
Solitary rectal ulcer syndrome is a rare and poorly understood disorder that can happen in people with long-lasting constipation. It can cause rectal bleeding, pain and straining when passing stool. Despite the name, sometimes more than one rectal ulcer develops in solitary rectal ulcer syndrome.
Solitary rectal ulcer syndrome may improve with simple lifestyle strategies, such as changing your diet and drinking more fluids. In severe cases, however, surgery may be needed.
Symptoms
Symptoms of solitary rectal ulcer syndrome include:
- Constipation.
- Rectal bleeding.
- Straining during bowel movements.
- Pain or a feeling of fullness in the pelvis or rectum.
- A feeling of incomplete passing of stool.
- Passing mucus from your rectum.
- Not being able to control bowel movements, called fecal incontinence.
However, some people with solitary rectal ulcer syndrome may experience no symptoms.
When to see a doctor
Make an appointment with a healthcare professional if you notice any symptoms that worry you.
Several other conditions may cause symptoms similar to those of solitary rectal ulcer syndrome. At your appointment, your healthcare professional may recommend tests and procedures to identify or rule out causes other than solitary rectal ulcer syndrome.
Causes
It's not always clear what causes solitary rectal ulcer syndrome. Researchers believe that stress or injury to the rectum may cause rectal ulcers to form.
Among the things that could injure the rectum are:
- Constipation or hardened stool in the rectum that's difficult to pass, called impacted stool.
- Straining when passing stool.
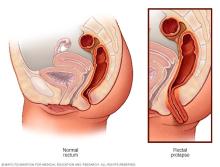
- A stretched rectum that comes out of the anus, known as rectal prolapse.
- Tightening of the pelvic floor muscles that slows blood flow to the rectum.
- Attempts to manually remove impacted stool.
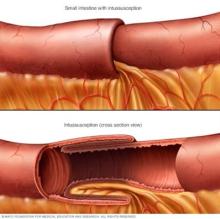
- One part of the intestine sliding inside another part, known as intussusception.
Risk factors
Though anyone can have solitary rectal ulcer syndrome, adults between the ages of 30 and 40 are most affected.
Diagnosis
One or more of the following tests may be used to diagnose solitary rectal ulcer syndrome:
- Sigmoidoscopy. During this test, a thin, flexible tube with a tiny camera is inserted into the rectum to examine the rectum and part of the colon. If a lesion is found, a tissue sample may be taken for laboratory testing. This is known as a biopsy.
- Anorectal manometry. Anorectal manometry is a test that evaluates bowel function. During the procedure, a flexible, tubelike device is inserted into the rectum. The response of anal and rectal muscles and nerves is then measured. Anorectal manometry is used to assess people with constipation, fecal incontinence and other disorders related to control of passing stool.
- Defecography. In defecography, a soft paste made of barium is inserted into the rectum. The barium paste is then passed in the stool while imaging is done. The barium shows up on X-rays and may reveal a prolapse or problems with muscle function and muscle coordination.
Specialized centers may offer magnetic resonance defecography. This test is done with a magnetic resonance imaging (MRI) machine and provides a 3D image of the rectum.
- Ultrasound. This imaging technique uses sound waves to create pictures. Your healthcare team may recommend an ultrasound to help differentiate solitary rectal ulcer syndrome from other conditions.
Treatment
Treatment for solitary rectal ulcer syndrome depends on the severity of the condition. People with mild symptoms may find relief through lifestyle changes, while people with more-severe symptoms may require medical or surgical treatment.
- Dietary changes. To relieve constipation, you may be given tips on increasing fiber in your diet.
- Behavior therapy. You may strain out of habit when passing stool. Behavior therapy can help you learn to relax your pelvic muscles when passing stool.
A behavioral technique called biofeedback can help lessen straining. In biofeedback, a specialist teaches you to control certain body responses that are not voluntary when passing stool, such as the tightening of your anus or pelvic floor muscles. Biofeedback may make you more aware of straining and help you control it.
- Medicines. Certain treatments such as topical steroids, sulfasalazine enemas, onabotulinumtoxinA (Botox) or argon plasma coagulation may help ease your rectal ulcer symptoms. However, these treatments don't work for everyone, and some are still considered experimental.
Surgical procedures used to treat solitary rectal ulcer syndrome include:
- Rectal prolapse surgery. If you have a rectal prolapse that's causing symptoms, a procedure called rectopexy may be recommended. Rectopexy secures the rectum in its anatomically correct position.
- Surgery to remove the rectum. An operation to remove the rectum may be an option if you have severe symptoms that haven't been helped by other treatments. The surgeon may connect the colon to an opening in the abdomen for waste to leave the body. This is called a colostomy. If you have a colostomy, a pouch or bag is attached to the abdomen to collect waste.
Self care
You can make changes to your daily life that may help relieve symptoms:
-
Increase the amount of fiber in your diet. Fiber adds bulk to your stool. The bulk helps push the contents of your intestines along so that they can be removed from the body when you pass stool. Depending on your age and sex, you should get between 22 and 34 grams of fiber a day. Ask your healthcare team about the right amount of fiber for you.
Nutrition labels on food packaging list the amount of fiber in a serving. The best sources of fiber are fruits, vegetables and whole grains. Eat fruits and vegetables with the skin on, and choose whole fruits and vegetables over juices. Look for breads and cereals that list whole wheat, oats or bran as the first ingredient.
- Try bulk laxatives and stool softeners. Bulk laxatives, such as psyllium husk (Metamucil, Natural Fiber Therapy, others) and calcium polycarbophil (FiberCon, Fiber-Lax, others), absorb fluid in the intestines and make stools bulkier. This helps trigger the bowel to contract and push stool out. However, take these products with water because they can cause obstruction.
Stool softeners, such as docusate (Colace, Surfak, others), help mix fluid into stools, making them easier to pass.
- Drink water throughout the day. Drinking enough water and other fluids helps keep your stool soft and easy to pass. Aim for 64 ounces (about 2 liters) of fluid a day unless you have restrictions due to other health conditions. For flavor and variety, you may want to add lemon juice to water. Or try other noncarbonated and caffeine-free beverages. Prune juice can be helpful because it has a natural laxative effect.
Preparing for your appointment
Start by seeing someone on your primary healthcare team if you have symptoms that worry you. If a health professional suspects that you may have solitary rectal ulcer syndrome, you may be referred to a doctor who specializes in the digestive system. This type of doctor is called a gastroenterologist.
What you can do
- Be aware of any pre-appointment restrictions. At the time you make the appointment, be sure to ask if there's anything you need to do in advance, such as restrict your diet.
- Write down key personal information, including any major stresses or recent life changes.
- Write down any symptoms you're experiencing, including any that may seem unrelated to the reason for which you scheduled the appointment.
- Make a list of all medicines, vitamins or supplements that you're taking.
- Write down questions to ask during your appointment.
For solitary rectal ulcer syndrome, some basic questions to ask include:
- What is likely causing my rectal ulcer symptoms?
- What are other possible causes for my symptoms?
- What kinds of tests do I need?
- Is my condition likely temporary or long lasting?
- Do I need treatment?
- What are my treatment options?
- How can I best manage other conditions I have while being treated for this condition?
- Do I need to follow any dietary or activity restrictions?
- Is there a generic alternative to the medicine you're prescribing me?
- Are there any brochures or other printed material that I can take with me?
- What websites do you recommend?
- Will I need follow-up visits? If so, how often?
What to expect from your doctor
You'll likely be asked a few questions during the appointment. If you've thought about your answers ahead of time, you may have a chance to go over any points you want to spend more time on.
You may be asked:
- When did you first begin having these symptoms?
- Have your symptoms been continuous or occasional?
- How severe are your symptoms?
- Have you recently had trouble with constipation?
- Does anything seem to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
© 1998-2026 Mayo Foundation for Medical Education and Research(MFMER). All rights reserved. Terms of Use
