Ventricular septal defect (VSD)
Conditions
Overview
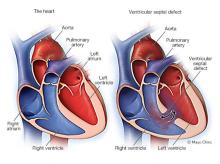
A ventricular septal defect (VSD) is a hole in the heart. It's a common heart problem present at birth (congenital heart defect). The hole occurs in the wall that separates the heart's lower chambers (ventricles).
A VSD changes how blood flows through the heart and lungs. Oxygen-rich blood gets pumped back to the lungs instead of out to the body. The oxygen-rich blood mixes with oxygen-poor blood. These changes may increase blood pressure in the lungs and require the heart to work harder to pump blood.
A small ventricular septal defect may cause no problems. Many small VSDs close on their own. Babies with medium or larger VSDs may need surgery early in life to prevent complications.
Symptoms
Symptoms of serious heart problems present at birth (congenital heart defects) often appear during the first few days, weeks or months of a child's life.
Symptoms of a ventricular septal defect (VSD) depend on the size of the hole and if there are any other heart problems. A small VSD may never cause symptoms.
In general, VSD symptoms in a baby may include:
- Poor eating
- Slow or no physical growth (failure to thrive)
- Fast breathing or breathlessness
- Easy tiring
- Whooshing sound when listening to the heart with a stethoscope (heart murmur)
Symptoms of a ventricular septal defect in adults may include:
- Shortness of breath, especially when exercising
- Whooshing sound when listening to the heart with a stethoscope (heart murmur)
When to see a doctor
Call your health care provider if your baby:
- Tires easily when eating or playing
- Is not gaining weight
- Becomes breathless when eating or crying
- Breathes rapidly or is short of breath
Call your provider if these symptoms develop:
- Shortness of breath
- Rapid or irregular heartbeat
- Fatigue or weakness
Causes
Ventricular septal defect (VSD) occurs as the baby's heart is developing during pregnancy. The muscular wall separating the heart into left and right sides doesn't form fully, leaving one or more holes. The size of the hole or holes can vary.
There's often no clear cause. Genetics and environmental factors may play a role. VSDs can occur alone or with other heart problems present at birth. Rarely, a ventricular septal defect can occur later in life after a heart attack or certain heart procedures.
How the heart works
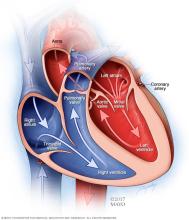
To understand more about ventricular septal defect (VSD), it may be helpful to know how the heart typically works.
The typical heart is made of four chambers — two upper chambers (atria) and two lower chambers (ventricles).
- The right side of the heart moves blood to the lungs.
- In the lungs, blood picks up oxygen.
- The lungs pump the oxygen-rich blood to the heart's left side.
- The left side of the heart pumps the oxygen-rich blood to the rest of the body.
A ventricular septal defect changes the direction of blood flow in the heart and lungs. The hole lets oxygen-rich blood go back into the lungs, instead of going out to the body. Oxygen-rich blood and oxygen-poor blood now mix together. If the ventricular septal defect is large, the blood pressure in the lung arteries may increase. The heart then must work harder to pump blood. A large VSD can also increase the amount of blood flow in the lung arteries, causing congestion.
Risk factors
Risk factors for ventricular septal defect include:
- Premature birth
- Down syndrome and other genetic conditions
- Family history of heart problems present at birth (congenital heart defects)
A baby born with ventricular septal defect may have other heart problems, such as:
- Atrial septal defect
- Coarctation of the aorta
- Double outlet syndrome
- Patent ductus arteriosus
- Tetralogy of Fallot
If you already have a child with a congenital heart defect, a genetic counselor can discuss the risk of your next child having one.
Complications
A small ventricular septal defect (VSD) may never cause any problems. Some medium or large VSDs may be life-threatening. Treatment can help prevent many complications.
Complications of ventricular septal defect can include:
- Heart failure. In a heart with a medium or large VSD, the heart works harder and the lungs have too much blood pumped to them. Without treatment, heart failure can develop.
- Eisenmenger syndrome. An unrepaired hole in the heart can lead to this complication after many years. Irregular blood flow causes the blood vessels in the lungs to become stiff and narrow. Blood pressure rises in the lungs' arteries (pulmonary hypertension). This syndrome permanently damages the blood vessels in the lungs.
- Endocarditis. This is a rare complication of VSD. An infection causes life-threatening inflammation of the inner lining of the heart's chambers and valves.
- Other heart problems. These include heart valve disease and irregular heart rhythms (arrhythmias).
Prevention
Because the cause is unclear, it may not be possible to prevent ventricular septal defect (VSD). But getting good prenatal care is important. If you have a VSD and are planning to become pregnant, schedule a visit with your health care provider and follow these steps:
- Get early prenatal care, even before you're pregnant. Talk to your provider before you get pregnant about your health and discuss any lifestyle changes that your doctor may recommend for a healthy pregnancy. Also, be sure you talk to your doctor about any medications you're taking.
- Take a multivitamin with folic acid. Taking 400 micrograms of folic acid daily has been shown to reduce birth defects in the brain and spinal cord. It may help reduce the risk of heart defects as well.
- Avoid alcohol. Drinking alcohol during pregnancy increases the risk of congenital heart defects.
- Don't smoke or use illegal drugs. If you smoke, quit. Smoking during pregnancy increases the risk of a congenital heart defect in the baby. Avoid using illegal drugs as they may harm a developing baby.
- Get recommended vaccinations. Be sure you're up to date on all of your vaccinations before becoming pregnant. Some infections can be harmful to a developing fetus. For example, having rubella (German measles) during pregnancy can cause problems in a baby's heart development. A blood test done before pregnancy can determine if you're immune to rubella. A vaccine is available for those who aren't immune.
- Keep diabetes under control. Careful control of blood sugar before and during pregnancy can reduce the risk of congenital heart defects in the baby. Diabetes that develops during pregnancy (gestational diabetes) generally doesn't increase a baby's risk. If you have diabetes, work with your provider to be sure it's well controlled before getting pregnant.
- Check with your provider before taking any medications. Some medications can cause birth defects. Tell your provider about all the medications you take, including those bought without a prescription.
If you have a family history of heart problems present at birth, consider talking with a genetic counselor and a heart doctor (cardiologist) before getting pregnant.
Diagnosis
Some ventricular septal defects (VSDs) are diagnosed soon after a child is born. However, VSDs may not be diagnosed until later in life. Sometimes a VSD can be detected by a pregnancy ultrasound before the baby is born.
If ventricular septal defect is present, the health care provider may hear a whooshing sound (heart murmur) when listening to the heart with a stethoscope.
Tests that are done to help diagnose ventricular septal defect include:
- Echocardiogram. This is the most commonly used test to diagnose a ventricular septal defect. Sound waves are used to create pictures of the heart in motion. An echocardiogram can show how well blood is moving through the heart and heart valves.
- Electrocardiogram (ECG). This quick and painless test records the electrical activity of the heart. It can show how fast or how slowly the heart is beating.
- Chest X-ray. A chest X-ray shows the condition of the heart and lungs. It can tell if the heart is enlarged and if the lungs have extra fluid.
- Pulse oximetry. A sensor placed on the fingertip records the amount of oxygen in the blood. Too little oxygen may be a sign of a heart or lung problem.
- Cardiac catheterization. In this test, a thin, flexible tube (catheter) is inserted into a blood vessel at the groin or arm and guided through the blood vessels into the heart. Through cardiac catheterization, doctors can diagnose congenital heart defects and determine the function of the heart valves and chambers.
- Cardiac magnetic resonance imaging (MRI) scan. Magnetic fields and radio waves are used to create detailed images of the heart. A health care provider might request this test if more information is needed after an echocardiogram.
- Computerized tomography (CT) scan. A series of X-rays create detailed images of the heart. It may be done if an echocardiogram didn't provide as much information as needed.
Treatment
Ventricular septal defect treatment may include regular health checkups, medications and surgery. Many babies born with a small ventricular septal defect (VSD) won't need surgery to close the hole. Some small VSDs close on their own.
If the VSD is small, regular health checkups may be all that's needed. Medication may be prescribed to treat any symptoms.
Babies who have large VSDs or who tire easily during feeding may need extra nutrition to help them grow. Some babies may require medication to help treat heart failure symptoms.
Medications
Medications won't repair a ventricular septal defect, but they may be given to treat symptoms or complications. The specific medications used depend on the symptoms and their cause. Water pills (diuretics) are used to decrease the amount of fluid in the body and reduce the strain on the heart.
Oxygen may be given.
Surgeries or other procedures
Surgery may be done if the VSD is medium or large or if it's causing severe symptoms. Babies who need surgery to repair the hole often have the procedure in their first year.
A surgeon may close small ventricular septal defects if their location in the heart could cause damage to nearby structures, such as the heart valves.
Surgeries and procedures to repair a ventricular septal defect include:
- Open-heart surgery. This is the preferred procedure for repairing most ventricular septal defects. A surgeon uses a patch or stitches to close the hole between the lower heart chambers. This type of VSD surgery requires a heart-lung machine and an incision in the chest.
- Catheter procedure. Some ventricular septal defects can be repaired using thin, flexible tubes (catheters) without the need for open-heart surgery. The health care provider inserts a catheter into a blood vessel, usually in the groin, and guides it to the heart. A small device is inserted through the catheter to close the hole.
After ventricular septal defect surgery, regular checkups are needed for life, ideally by a heart doctor (cardiologist). Checkups often include imaging tests to determine how well surgery is working.
Self care
Lifestyle changes may be recommended to keep the heart healthy and prevent complications.
-
Prevent heart infections. Sometimes heart problems can increase the risk of infection in the lining of the heart or heart valves (endocarditis). Antibiotics may be recommended before dental procedures if you have low oxygen due to a large VSD. The medicines may also be recommended if you have a surgically repaired VSD with a patch that still has some blood flow across it. Antibiotics may also be recommended if you recently had catheter-based VSD repair.
For most people with a ventricular septal defect, good oral hygiene and regular dental checkups can prevent endocarditis.
- Ask about exercise restrictions. Many people with a ventricular septal defect can lead healthy, active lives without restrictions. But some may need to limit exercise and sports activities. Ask your health care provider which sports and types of exercise are safe for you or your child. People with Eisenmenger syndrome should avoid strenuous physical activity.
-
Talk to your provider before getting pregnant. If you have a ventricular septal defect and are pregnant or hoping to be, talk to your health care provider about the possible risks and complications. Together you can discuss and plan for any special care needed during pregnancy.
A small VSD or a repaired one without complications doesn't pose a large additional pregnancy risk. However, a large, unrepaired VSD, irregular heart rhythms, heart failure or pulmonary hypertension increase the risk for pregnancy complications.
Pregnancy is considered very high risk for those with Eisenmenger syndrome and is not recommended.
Coping and support
You may find that talking with others who've experienced similar events or situations can be helpful. Support groups offer parents, families and caregivers a place to share concerns and find encouragement. Ask your health care provider if there are any support groups in your area.
Preparing for your appointment
If a baby has a large ventricular septal defect, it will likely be diagnosed soon after birth. Sometimes it's diagnosed before birth during a pregnancy ultrasound.
If you think your child has a VSD that wasn't recognized at birth, make an appointment with your child's health care provider. You may be referred to a heart doctor (cardiologist).
Here's some information to help you prepare for your appointment.
What you can do
Write down the following and bring the notes with you to the appointment:
- Any symptoms, including any that may seem unrelated to heart problems.
- When the symptoms started and how often they occur.
- Important medical information, including a family history of heart problems present at birth.
- All medications, including those bought without a prescription. Include dosages.
- Questions to ask the health care provider.
Ask a family member or friend to come with you to the appointment, if possible. Someone who goes with you can help remember what the care provider says.
Preparing a list of questions can help you and your health care provider make the most of your time together. Questions to ask the provider at the first appointment include:
- What is likely causing these symptoms?
- Are there other possible causes?
- What tests are needed? Is any special preparation needed?
- Should a specialist be consulted?
- Are there any brochures or other printed material I can take home with me? What websites do you recommend?
Questions to ask if you are referred to a heart doctor (cardiologist) include:
- How large is the hole in the heart?
- What is the risk of complications from this condition?
- How can we monitor for complications?
- What treatment do you recommend?
- How often should we schedule follow-up exams and tests?
- What is the long-term outlook for this condition?
- Are there any activity restrictions?
Don't hesitate to ask other questions.
What to expect from your doctor
Your health care provider is likely to ask many questions, including:
If you are the person affected:
- What are the symptoms?
- When did the symptoms begin?
- Have the symptoms gotten worse over time?
- Are you aware of heart problems in your family?
- Are you being treated, or have you recently been treated, for other health conditions?
- Are you planning to become pregnant?
If your baby or child is affected:
- Does your child tire easily while eating or playing?
- Is your child gaining weight?
- Does your child breathe rapidly or run out of breath when eating or crying?
- Has your child been diagnosed with other medical conditions?
© 1998-2026 Mayo Foundation for Medical Education and Research(MFMER). All rights reserved. Terms of Use
