Whipple's disease
Conditions
Overview
Whipple disease is a rare infection caused by bacteria that keeps food from being digested well. It affects the breakdown of food and keeps the body from taking in nutrients.
Whipple disease most often affects the joints and digestive system. The bacteria that cause Whipple disease also can infect other organs, including the brain, heart and eyes.
Without treatment, Whipple disease can be serious or even deadly. But antibiotics can treat Whipple disease.
Symptoms
The main symptoms of Whipple disease often include:
- Loose stools.
- Stomach cramping and pain, which may get worse after meals.
- Weight loss due to the body not taking in nutrients.
- Joint pain.
Joint pain may be one of the first symptoms of Whipple disease. Digestive symptoms often don't start until later.
Other symptoms linked with Whipple disease include:
- Fever.
- Cough.
- Large lymph nodes.
- Darker skin in scars and in areas that get sun. Skin darkening may be harder to see on Black or brown skin.
- Chest pain.
- Tiredness.
- Weakness.
- Anemia, which means not having enough healthy red blood cells to carry oxygen through the body.
Brain and nervous system symptoms, also called neurological symptoms, may include:
- Trouble walking.
- Vision issues, including not being able to control eye movements.
- Confusion.
- Memory loss.
Symptoms tend to happen slowly over years in most people with this condition. In some people, symptoms such as joint pain and weight loss happen years before the digestive symptoms that lead to diagnosis.
When to see a doctor
Whipple disease can be life-threatening, but most often it's treatable. Call your healthcare professional if you are losing weight without trying or have joint pain.
Causes
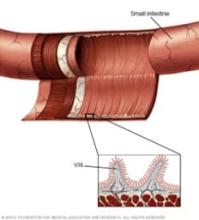
A type of bacterium called Tropheryma whipplei causes Whipple disease. These germs affect the lining of the small intestine first. They form small sores, also called lesions, in the wall of the intestine. The bacteria also harm the fine, hairlike structures called villi that line the small intestine.
Experts don't know how the bacteria spread to humans. Not all people exposed to the bacteria get Whipple disease. Some researchers believe that people with the condition may have genetic change that affects their immune system and makes them more likely to get sick from the bacteria.
Risk factors
Because experts know so little about the bacteria that cause Whipple disease, there are no clear risk factors for the condition. Whipple disease seems to be more likely to affect:
- Men ages 30 to 60.
- White people in North America and Europe.
- People who work with or near soil or animals, such as farmers and other people who work outdoors and often are near sewage and wastewater.
Complications
Whipple disease gets worse over time. It can be deadly. Late diagnosis and treatment can cause the infection to spread to the central nervous system, which can cause lasting harm.
Diagnosis
Diagnosing Whipple disease most often involves a physical exam. Because symptoms are like those of other conditions, your healthcare professional first rules out other more common causes.
Tests for Whipple disease may include a biopsy, a lumbar puncture or blood tests.
Biopsy
Your healthcare professional passes a thin tube with a camera, called a scope, through your mouth into your small intestine. Through the scope, your healthcare professional takes tissue samples from the small intestine for study under a microscope.
If these tissue samples don't confirm the diagnosis, your healthcare professional might take a tissue sample from an enlarged lymph node or do other tests.
Lumbar puncture
Also called a spinal tap, this test involves a thin needle put into the back to take a small amount of fluid from the spine. The fluid is called cerebrospinal fluid. The sample goes to a lab for study.
A DNA-based test known as a polymerase chain reaction (PCR) test can find the bacteria that cause Whipple disease in spinal fluid samples or in biopsy samples. Some medical centers offer this test.
Blood tests
Your healthcare professional also may order blood tests, such as a complete blood count. Blood tests can find certain conditions linked with Whipple disease. For instance, a blood test can find anemia, which means you have too few red blood cells.
Treatment
Treatment of Whipple disease is with one antibiotic or a mix of antibiotics. These medicines kill the bacteria that cause the infection.
Treatment is long-term. It may take a year or two to kill the bacteria. But symptom relief most often comes much quicker, within the first week or two. Most people with no brain or nervous system complications recover fully after a course of antibiotics.
Healthcare professionals often choose antibiotics that can wipe out infections in the small intestine and cross the layer of tissue around your brain, called the blood-brain barrier. These antibiotics kill bacteria that may have gone into your brain and central nervous system.
Because you take antibiotics for a long time, your healthcare professional watches your condition to see if it stops responding to the medicine. If your condition gets worse during treatment, you may need to take another antibiotic.
Treatment for basic Whipple disease
Most often, Whipple disease therapy begins with 2 to 4 weeks of the antibiotics ceftriaxone or penicillin given through a vein in your arm. After that, you may take sulfamethoxazole-trimethoprim (Bactrim, Septra) by mouth for 1 to 2 years.
Possible side effects of ceftriaxone and sulfamethoxazole-trimethoprim include allergic reactions, loose stools or upset stomach and vomiting.
Other medicines a healthcare professional might prescribe include oral doxycycline (Acticlate, Doryx) with the antimalarial medicine hydroxychloroquine (Plaquenil, Sovuna). You may need to take these for 1 to 2 years as well.
Possible side effects of doxycycline include not wanting to eat, upset stomach, vomiting and sensitivity to sunlight. Hydroxychloroquine may cause not wanting to eat, loose stools, headache, stomach cramps and dizziness.
Symptom relief
Your symptoms should improve within 1 to 2 weeks of starting antibiotic treatment and go away within about one month.
Even though symptoms improve quickly, lab tests may show that you still have the bacteria for two or more years after starting antibiotics. Follow-up testing helps your healthcare professional know when you can stop taking antibiotics. If your symptoms aren't getting better, follow-up testing can show whether the medicine you take has stopped working.
Even after treatment that works, Whipple disease can come back. If that happens, you need to repeat antibiotic therapy.
Taking supplements
Because Whipple disease can keep your body from taking in nutrients, your healthcare professional may suggest that you take vitamin and mineral supplements to make sure you get the nutrition you need. You may need to take vitamin D, folic acid, calcium, iron and magnesium.
Preparing for your appointment
If you have symptoms that might be Whipple disease, see your healthcare professional. An early diagnosis cuts the risk of serious health effects linked with not treating the condition.
A healthcare professional who isn't sure about the diagnosis may send you to a doctor who specializes in infectious diseases.
Here's some information to help you get ready for your appointment.
What you can do
Ask a family member or friend to go with you to the appointment. Someone who's with you can help you remember the information you get.
Make a list of:
- Your symptoms, including when they began and how they may have changed over time. Include symptoms that don't seem linked to the reason you made the appointment.
- Key medical information, including other conditions you have. Also list medicines, vitamins and supplements you take, including dosages.
- Key personal information, including any recent changes or stressors in your life. These may be linked to digestive symptoms.
- Questions to ask your healthcare professional.
Some basic questions to ask include:
- What is the most likely cause of my condition?
- What tests do I need?
- What treatment do you suggest?
- I have other medical conditions. How can I manage them together?
- When might my symptoms get better with treatment?
- How long will I need to take medicines?
- How often will you need to see me during treatment?
- Should I take vitamins or supplements?
Be sure to ask all the questions you have.
What to expect from your doctor
Your healthcare professional is likely to ask you questions, such as:
- Do your symptoms get worse after a meal?
- Have you lost weight without trying?
- Do your joints hurt?
- Have you noticed issues with your eyes?
- Has anyone close to you had symptoms like yours recently?
- Do you have any family history of bowel conditions or colon cancer?
- Are you allergic to any medicines?
© 1998-2026 Mayo Foundation for Medical Education and Research(MFMER). All rights reserved. Terms of Use
