Zenker's diverticulum
Conditions
Overview
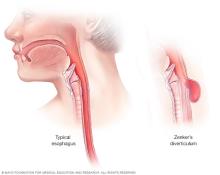
In Zenker's diverticulum, a bulge or pouch forms at the top of the tube that connects the throat to the stomach, called the esophagus. The condition is not common. Connected bands of muscle that work to pass food from the mouth to the stomach make up the esophagus.
Over time, the bulge of Zenker's diverticulum can get bigger. Food, pills and even thick mucus can get stuck in the pouch instead of going through the esophagus. This can lead to problems with eating and other complications.
The cause of Zenker's diverticulum is not known. It happens most often to men older than 60. Treatment for symptoms of Zenker's diverticulum often is surgery.
Symptoms
A small Zenker's diverticulum may not have any symptoms. But the bulge may get bigger over time. It can trap food, mucus and pills. Symptoms might include:
- Trouble swallowing, called dysphagia.
- Burping.
- A gurgling noise at the back of the throat.
- Coughing.
- Hoarseness.
- Bad breath.
- Choking.
If the pouch gets big enough, what's in it may spill into the throat. Then Zenker's diverticulum symptoms might include:
- Feeling of food stuck in the throat.
- Coughing up or spitting up food 1 to 2 hours after eating. This is called regurgitation.
- Breathing food into the lungs, called aspirating.
Causes
The cause of Zenker's diverticulum isn't known. It's not known why the walls of the esophagus change to form a bulge or pouch in the condition.
The cause of Zenker's diverticulum might involve the muscles of the esophagus not working together. Most often, a muscle at the top of the esophagus relaxes to let the food down. If that doesn't happen, food can get trapped in the esophagus.
If the muscle in the area where the food gets trapped is weak, the food can cause the esophagus to bulge and form a pouch.
Risk factors
Risk factors for Zenker's diverticulum include:
- Being older than 60.
- Being male.
- Having gastroesophageal reflux disease (GERD) or a condition in which part of the stomach bulges into the chest, called a hiatal hernia.
- Having spinal surgery.
Complications
Complications can happen if Zenker's diverticulum isn't treated. The bulge of Zenker's diverticulum can get larger if it's not treated. Complications of Zenker's diverticulum can include:
- Lung infection. Breathing in food, called aspirating, can lead to a lung infection. This is called aspiration pneumonia.
- Weight loss and not getting enough nutrients, called malnutrition. Trouble swallowing can lead to weight loss and malnutrition.
Diagnosis
To diagnose Zenker's diverticulum, a healthcare professional, often an ear, nose and throat (ENT) specialist, does a physical exam and asks about your symptoms.
Tests
The test most often done to diagnose Zenker's diverticulum is a barium swallow. In this test, a specialist takes a series of X-rays of the digestive tract after you swallow a liquid that coats the walls of the digestive tract. The liquid, called barium sulfate, makes the digestive tract easier to see on X-ray.
Treatment
To treat Zenker's diverticulum, surgery or other procedures may be needed. Eating softer foods in smaller bites might help with swallowing if you have mild symptoms of Zenker's diverticulum. Your healthcare professional might suggest a dietician to help you learn what to eat.
Types of surgeries or other procedures
Repairing the esophagus with a procedure or surgery is the most common treatment for Zenker's diverticulum that's causing symptoms. Often, ear, nose and throat conditions (ENT) specialists do the procedure or surgery. They often do the procedure through a tube called an endoscope that goes into the mouth to the esophagus. This is less invasive than open surgery.
Endoscope procedures to repair Zenker's diverticulum, sometimes called endoscopic repairs, most often have shorter surgery times and may have a shorter hospital stay compared to open surgery. They also often have similar results and improve Zenker's diverticulum symptoms for people as much as open surgery. But people who have endoscope procedures might have a higher risk of a Zenker's diverticulum coming back.
There are two main types of endoscope procedures used to repair Zenker's diverticulum. They each take about 1 to 2 hours to do.
-
Rigid endoscope procedure. Before the procedure, you're given medicine called general anesthesia to put you into a sleeplike state. The ENT specialist uses a rigid endoscope to get to the esophagus. A rigid endoscope doesn't bend or twist. The ENT specialist often uses a laser or may use a stapler to widen the opening to the bulge.
Sometimes, the ENT specialist can remove the pouch with the laser device. This is called an endoscopic diverticulectomy. Electrocautery is another choice, but it's rarely used with the rigid endoscope procedure.
- Flexible endoscope procedure. Before this procedure, you may get medicine that causes a near sleeplike state, called deep sedation, or general anesthesia. The endoscope is flexible. A surgeon uses an electric current, called electrocautery, to cut the bulge. Clips may be used for any bleeding.
Repairing Zenker's diverticulum sometimes may need to be done in an open surgery, sometimes called an open repair. Before the procedure, you're given general anesthesia. The ENT specialist makes a cut, called an incision, in the neck to remove the bulge.
This surgery most often takes 2 to 3 hours. People who have this type of surgery often stay in the hospital for one or more days. This surgery eases symptoms for most people.
Possible complications
Possible complications of surgery to repair Zenker's diverticulum may include:
- Infection.
- Blood clots.
- Reactions to anesthesia.
- A hole in the esophagus.
- Dental injury such as a chipped tooth when surgery is done using an endoscope.
Results
Both endoscopic and open surgery ease Zenker's diverticulum symptoms for most people. Endoscope procedures most often have shorter surgery times. Hospital stays often are just one night for endoscopic and open surgeries.
Open surgery leaves a small scar in the neck. Open surgery also can have a bit higher risk of a hole in the esophagus compared to endoscopic techniques. For a large Zenker's diverticulum, open surgery may be the best choice for full removal of the pouch.
If the first procedure doesn't ease symptoms or if Zenker's diverticulum comes back, you may need another procedure. And if Zenker's diverticulum comes back, it often has no symptoms. Researchers study newer ways of fixing the condition.
Preparing for an appointment
If you have trouble swallowing or other symptoms of Zenker's diverticulum, make an appointment with your primary healthcare professional. You may be sent to a specialist in illnesses of the ear, nose and throat, called an otolaryngologist or ear, nose and throat specialist (ENT).
Here's some information to help you get ready for your appointment.
What you can do
When you make the appointment, ask if there's anything you need to do in advance, such as fasting before having a certain test. Make a list of:
- Your symptoms, including any that seem unrelated to the reason for your appointment, and when they began.
- Key personal information, including major stresses, recent life changes and family medical history.
- All medicines, vitamins or other supplements you take, including doses.
- Questions to ask your healthcare professional.
Take a family member or friend along, if possible, to help you remember the information you get.
For Zenker's diverticulum, basic questions to ask include:
- What's likely causing my symptoms?
- What tests do I need?
- Is my condition likely to go away or be long lasting?
- What's the best course of action?
- I have these other health conditions. How can I best manage them together?
- Are there restrictions I need to follow?
- Should I see a specialist?
- Are there brochures or other printed material I can have? What websites do you suggest?
Be sure to ask all the questions you have.
What to expect from your doctor
Your healthcare professional is likely to ask you questions, such as:
- Have your symptoms been ongoing or do they come and go?
- How severe are your symptoms?
- What, if anything, seems to make your symptoms better?
- What, if anything, seems to make your symptoms worse?
What you can do in the meantime
If you have trouble swallowing, try eating softer foods and taking smaller bites.
© 1998-2026 Mayo Foundation for Medical Education and Research(MFMER). All rights reserved. Terms of Use
