Colonoscopy
Procedures
Overview
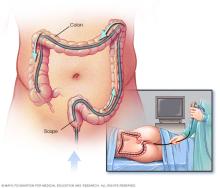
A colonoscopy (koe-lun-OS-kuh-pee) is a procedure used to examine the inside of the colon, rectum and when indicated the end of the small intestine. It can investigate symptoms such as bleeding from the anus, changes in bowel movements or belly pain. It can help detect conditions that affect the colon, including colorectal cancer, inflammatory bowel disease (IBD) and diverticular disease.
Colonoscopy also is commonly done to screen for colorectal cancer even when there are no symptoms. During the exam, colon polyps, which are precancerous mounds of tissue, may be detected. Removal of these polyps can help prevent the risk of developing colorectal cancer. Colonoscopy is considered one of the most comprehensive methods for colorectal cancer screening because it allows a healthcare professional to examine the entire colon and remove polyps during the same procedure.
During a colonoscopy, a long, flexible tube called a colonoscope is placed into the rectum and guided through the colon. A small video camera at the tip of the colonoscope sends images to a monitor, allowing the health professional to closely examine the lining of the colon. Tissue samples, called biopsies, also may be taken and sent to a laboratory for further evaluation.
Why it's done
Your healthcare professional may recommend a colonoscopy to:
-
Investigate intestinal signs and symptoms. A colonoscopy can help evaluate possible causes of symptoms such as abdominal pain, rectal bleeding, long-lasting diarrhea or changes in bowel habits related to some conditions that affect the colon. These include colorectal cancer, polyps, diverticular disease and inflammatory bowel disease, such as ulcerative colitis or Crohn's disease. It also may be used to evaluate irregularities seen on imaging studies.
Colonoscopy is not used to diagnose irritable bowel syndrome (IBS), celiac disease or hernias.
-
Screen for colorectal cancer. For people at average risk of colon cancer, colorectal cancer screening is recommended to start at age 45. Colonoscopy is one screening option. It may be repeated every 10 years when findings do not require earlier follow-up.
People with risk factors may need to start screening earlier than age 45 or be screened more often. Risk factors include:
- A family history of colorectal cancer or polyps.
- Inflammatory bowel disease, such as ulcerative colitis or Crohn's disease.
- Inherited genetic syndromes, such as Lynch syndrome or familial adenomatous polyposis (FAP).
Colonoscopy is one of several screening options. The choice of test depends on individual risk factors and preferences.
- Monitor for polyps. If polyps have been found before, follow-up colonoscopy may be recommended to look for and remove additional polyps. This can help reduce the risk of colorectal cancer.
- Treat certain conditions. In some cases, colonoscopy may be used for treatment, such as removing growths, relieving a blockage or retrieving an object from the colon.
Referral requirements for colonoscopy vary. Check with your healthcare professional or insurance provider to find out whether you need a referral.
Colonoscopy compared with other tests
A colonoscopy examines the entire colon and rectum and allows polyps to be removed during the same procedure. Depending on your situation, other procedures may be used to examine the digestive system.
An upper endoscopy examines the esophagus, stomach and upper small intestine. It is not used to evaluate the colon or screen for colorectal cancer.
At-home stool tests such as Cologuard or the fecal immunochemical test (FIT) analyze a stool sample for signs of colorectal cancer or advanced polyps. But they do not examine the colon directly or remove polyps. A positive stool test result requires follow-up with a colonoscopy. There is no such thing as an at-home colonoscopy.
A sigmoidoscopy examines only the lower part of the colon and rectum. A colonoscopy examines the entire colon. Findings during sigmoidoscopy may require follow-up with a colonoscopy.
Risks
Colonoscopy is generally considered safe, but complications can happen.
Possible risks include:
- Bleeding, which most often occurs after removal of a polyp or when a tissue sample is taken.
- A tear in the wall of the colon, called perforation, which may need further treatment or surgery.
- Reactions to sedation, including breathing or heart-related problems, particularly in older adults or people with underlying medical conditions.
How you prepare
Before a colonoscopy, you'll need to empty your colon with a bowel preparation so the lining of the colon and rectum can be clearly seen during the exam.
Preparation usually begins 1 to 2 days before the procedure, depending on the type of bowel preparation recommended.
To prepare for a colonoscopy, your healthcare professional may ask you to:
-
Follow a special diet. In the days before the procedure, you may be asked to follow a low-fiber or low-residue diet. These diets limit foods that leave material in the colon. These foods include whole grains, nuts, seeds, and raw fruits or vegetables.
The day before the colonoscopy, you typically stop eating solid food and follow a clear liquid diet. Clear liquids may include water, tea or coffee without milk or cream. They also include broth and clear carbonated beverages. Do not drink red liquids because they can be mistaken for blood during the exam. You may be told to stop drinking liquids several hours before the procedure.
-
Adjust your medicines. Tell your healthcare professional about all medicines and supplements you take, especially if you have diabetes, high blood pressure or heart disease or take iron supplements.
Blood-thinning medicines may need to be adjusted or temporarily stopped before the procedure. They include aspirin, anticoagulants and medicines that affect platelets.
-
Take a bowel preparation. Bowel preparation is used to clear stool from the colon and is often started the evening before the procedure. Some regimens require doses both the night before and the morning of the exam.
Types of bowel preparation include:
- Liquid laxatives, which are the most commonly used preparations and involve drinking a prescribed solution that causes frequent bowel movements. These are often taken as a split dose. You take one part the evening before and another part the morning of the procedure.
- Pill-based preparations, which use tablets taken with clear liquids to cleanse the colon. These may be an option for some people who cannot tolerate large volumes of liquid.
- Magnesium citrate-based preparations, which may be used in selected situations but are not right for everyone, particularly people with kidney, heart or fluid-balance conditions.
Bowel preparation usually begins to work within a few hours after you start taking it. The timing can vary depending on the type of preparation used and individual factors.
Stool typically changes from solid to loose and then becomes watery and light colored or clear as the colon empties. This change usually indicates that the bowel preparation is working as intended. Most people have frequent bowel movements over several hours, especially after each dose, as stool is cleared from the colon. It is important to complete the entire bowel preparation as instructed, even if stool appears clear before all doses are finished.
If you cannot finish the bowel preparation
If you are having a hard time drinking the entire bowel preparation or keeping it down, contact your healthcare professional for instructions.
If you cannot finish the bowel preparation as instructed, the colon may not be adequately cleared, which can make it difficult to examine the colon. This may require the procedure to be delayed or repeated.
Your healthcare professional may recommend changes to the preparation or reschedule the colonoscopy to ensure the exam can be completed safely and effectively.
Special situations
Certain situations may affect how a colonoscopy is scheduled or performed, so it is important to discuss these with your healthcare professional before the procedure.
- Pregnancy. Colonoscopy during pregnancy is generally avoided unless there is a strong medical reason for it and the potential benefits outweigh the risks. It is usually scheduled for the second trimester when possible. Healthcare teams take special precautions related to sedation, positioning and monitoring.
- Menstrual period. You can have a colonoscopy during your menstrual period. Menstruation does not interfere with the procedure or its accuracy.
What you can expect
During the procedure
A colonoscopy usually is performed by a doctor who specializes in conditions of the digestive system, called a gastroenterologist. In some settings, a surgeon with specialized training in endoscopic procedures may perform colonoscopy.
During a colonoscopy, you wear a gown, but likely nothing else. You need to remove underwear. Usually, sedation or anesthesia is recommended. Most colonoscopies are performed using sedation given through a vein to help you relax and reduce discomfort during the procedure. Sedation may range from moderate sedation to deep sedation. In some situations, general anesthesia may be used based on individual factors.
A colonoscopy is usually not painful because sedation is commonly used. The exam begins with you on your side on the exam table, usually with your knees drawn toward your chest. The doctor inserts a colonoscope into your rectum. When the scope is moved or air is introduced, you may feel stomach cramping or the urge to have a bowel movement. This depends on your level of sedation.
The scope — which is long enough to reach the entire length of your colon — contains a light and a tube that allows the doctor to pump air, carbon dioxide or water into your colon. The air or carbon dioxide inflates the colon, which provides a better view of the lining of the colon. The scope contains a tiny video camera at its tip. The camera sends images to an external monitor so that the doctor can study the inside of your colon.
The doctor also can insert instruments through the tube to take tissue samples, called biopsies, or remove polyps or other areas of tissue.
A colonoscopy typically takes about 30 to 60 minutes.
After the procedure
After the colonoscopy, you are taken to a recovery area. Your healthcare team monitors you for about an hour.
After sedation
Because sedation can affect judgment and coordination, you need someone to take you home. You may be told not to drive, return to work or make important decisions for the rest of the day.
Discomfort
It is typical to feel bloated, have gas pains and pass large amounts of air after a colonoscopy. Walking can help relieve these side effects. Your healthcare team may recommend a common pain reliever such as acetaminophen (Tylenol, others). But do not take aspirin.
Diet after a colonoscopy
Most people can return to eating soon after the procedure. Your healthcare professional may recommend starting with light or easy-to-digest foods, especially if you feel bloated or nauseated.
Recovery time
Most people return to their usual level of activity by the next day. Recovery time can vary depending on the type of sedation used and whether tissue samples were taken or polyps were removed.
Results
Your healthcare professional reviews the findings from your colonoscopy and shares the results with you. You may receive some information the same day as the procedure. Laboratory results for tissue samples may take a few days.
Healthcare professionals may describe colonoscopy results using terms such as negative or positive. A negative result means no polyps or tissue changes were found. A positive result means polyps or tissue changes were seen and may need follow-up.
When no polyps or tissue changes are found
If no polyps or tissue changes are seen, your healthcare professional may recommend another colonoscopy in the future based on your age and risk factors.
You may be advised to have another colonoscopy:
- In 10 years if you are at average risk of colon cancer and no findings were seen.
- In 7 to 10 years if only one or two small polyps with low-risk features were removed.
- In 1 to 5 years, if you have factors that increase your risk, such as a personal history of polyps, certain genetic conditions or a family history of colon cancer.
If stool in the colon prevented a full exam, your healthcare professional may recommend repeating the colonoscopy sooner. The timing depends on how much of the colon could be seen. A different bowel preparation may be suggested before the next exam.
When polyps or tissue changes are found
If polyps or other tissue changes are found, they are often removed during the procedure and sent to a laboratory for testing. Most polyps are not cancer, but some may develop into cancer over time.
The timing of future colonoscopy depends on your results and risk factors.
Your healthcare professional may recommend another colonoscopy sooner if:
- More than two polyps were found.
- A polyp larger than about 1 centimeter (about 1/3 inch) was removed.
- Laboratory testing shows features linked with a higher risk of future cancer.
- A cancerous polyp was found.
If a polyp or area of tissue could not be removed during the exam, you may be referred to a specialist with experience removing large polyps. Or you may be advised to have surgery.
Problems with your exam
If the view through the scope was limited, your healthcare professional may recommend repeating the colonoscopy or scheduling the next exam sooner. If the scope could not be passed through the entire colon, a virtual colonoscopy may be recommended to examine the remaining area.
© 1998-2026 Mayo Foundation for Medical Education and Research(MFMER). All rights reserved. Terms of Use
