Chronic kidney disease
Conditions
Overview
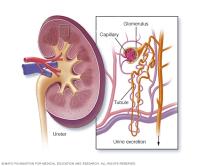
Chronic kidney disease happens when the kidneys are damaged for more than a few months. The kidneys clean the blood by removing waste and extra fluid, which leaves the body as urine. They help control blood pressure and balance salt and minerals. The kidneys also help the body make red blood cells and keep bones strong.
In the early stages of chronic kidney disease, you might not feel sick or have any symptoms. You might not know that you have kidney disease until the condition is advanced.
Healthcare professionals can find kidney disease through blood and urine tests. These tests look for high levels of waste in the blood or unusual things in the urine, such as protein or tiny amounts of blood. They also might use tests such as ultrasound or CT scans to look at the kidneys.
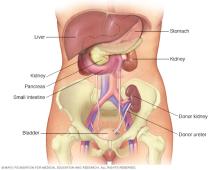
Treatment for chronic kidney disease aims to slow down damage to the kidneys. This often is done by managing the cause of the damage. But, even after a cause has been found and treated, kidney damage could still get worse. Chronic kidney disease can progress to end-stage kidney failure. This is fatal unless a person gets a kidney transplant or starts dialysis, a treatment that does the job of the kidneys.
Symptoms
Chronic kidney disease symptoms tend to develop slowly over time.
Loss of kidney function can cause a buildup of fluid or waste in the body. It also can cause acids, potassium and phosphate to build up in the blood.
Symptoms of kidney disease often are vague. Most people with kidney disease have no symptoms until the very last stages of kidney disease. This is known as advanced kidney disease.
When chronic kidney disease becomes advanced, loss of kidney function can cause:
- Nausea.
- Vomiting.
- Loss of appetite.
- Fatigue and weakness.
- Sleep problems.
- Decreased mental sharpness.
- High blood pressure that's hard to manage.
- Shortness of breath, if fluid builds up in the lungs.
Stages of kidney disease
There are five stages of kidney disease. To learn what stage you have, your healthcare team performs a blood test to check how well the kidneys are working. This blood test is called the estimated glomerular filtration rate (eGFR). The eGFR measures how much blood the kidneys filter each minute, recorded as milliliters per minute (mL/min). A low eGFR number means the kidneys are working less well.
When the kidneys no longer work at the level needed to keep a person alive, it's called end-stage kidney disease. This happens when you have an eGFR under 15.
As a part of kidney disease staging, your healthcare professional also might test whether you have protein in your urine.
| Kidney disease stage | eGFR, mL/min | Kidney function | ||
|---|---|---|---|---|
| Stage 1 | 90 or above | Healthy kidney function | ||
| Stage 2 | 60 to 89 | Mild loss of kidney function | ||
| Stage 3a | 45 to 59 | Mild to moderate loss of kidney function | ||
| Stage 3b | 30 to 44 | Moderate to severe loss of kidney function | ||
| Stage 4 | 15 to 29 | Severe loss of kidney function | ||
| Stage 5 | Less than 15 | Kidney failure | ||
| Source: National Kidney Foundation | ||||
When to see a doctor
If you have an ongoing health condition that raises your risk of kidney disease, your main healthcare professional may want to monitor the health of your kidneys. Having long-standing high blood pressure, diabetes or an autoimmune disease such as lupus can cause damage to the kidneys.
Regular checkups to monitor how well the kidneys are working may include blood tests and tests to check for protein in the urine. You may see your main healthcare professional every 6 to 12 months for these tests. If test results show possible kidney problems, you may be referred to a doctor who specializes in kidney diseases. This type of doctor is called a nephrologist.
Causes
Chronic kidney disease happens when a disease or condition hurts kidney function. Often, chronic kidney disease has more than one cause.
Causes of chronic kidney disease include:
- Type 1 or type 2 diabetes.
- High blood pressure.
- Some autoimmune diseases, such as lupus, sarcoidosis and Sjogren syndrome.
- Polycystic kidney disease or other inherited kidney diseases.
- Prolonged obstruction of the urinary tract, from conditions such as enlarged prostate or urinary tract tumors.
- Vesicoureteral (ves-ih-koe-yoo-REE-tur-ul) reflux, a condition that causes urine to back up into the kidneys.
- Certain medicines, such as lithium, large doses of ibuprofen or other nonsteroidal anti-inflammatory drugs, and drugs that suppress the immune system.
Risk factors
Factors that can raise your risk of chronic kidney disease include:
- Diabetes.
- High blood pressure.
- Heart disease.
- Smoking.
- Being overweight.
- Being Black, Native American or Asian American.
- Family history of kidney disease.
- Changes or problems in the shape or size of the kidneys.
- Older age.
- Frequent use of medicines that can damage the kidneys.
Complications
Chronic kidney disease can affect almost every part of the body. Complications can include:
- High blood pressure. Since the kidneys don't work as well to remove extra salt and water from the body, blood pressure starts to rise. High blood pressure can lead to more kidney damage, which in turn raises blood pressure even more.
- Acid buildup. Also called acidosis, acid buildup happens when the kidney can't remove extra acids the body makes or you take in with the foods you eat. This can lead to issues with bone health and protein breakdown.
- Fluid retention. This could lead to leg swelling, high blood pressure or fluid in the lungs, also called pulmonary edema, which causes shortness of breath. Fluid retention usually happens in later stages of kidney disease. A sudden increase in body weight might be a sign of fluid retention.
- High blood potassium levels. Also called hyperkalemia, this condition may happen suddenly. It usually happens in the later stages of kidney disease and may damage the heart and be life-threatening.
- Anemia. This happens when there aren't enough healthy red blood cells to carry oxygen to the body's tissues.
- Heart disease. With advanced kidney disease, blood vessels called arteries can become stiff and get clogged. This makes blood pressure go up and could lead to heart disease.
- Weak bones. Weak bones and a higher risk of bone fractures can happen.
- Sexual health concerns. Lower sex drive, erectile dysfunction or reduced fertility can happen.
- Damage to the central nervous system. This could lead to trouble concentrating or personality changes. This complication usually happens in the very last stages of kidney disease.
- Immune system changes. You may have a lowered immune response, which puts you at risk of infection.
- Pericarditis. This inflammation of the saclike membrane that covers the heart can happen in people with advanced kidney disease.
- Pregnancy complications. The mother and the unborn baby may be at risk.
- Lasting damage to the kidneys. Dialysis or a kidney transplant may be needed to survive.
Prevention
To lower the risk of developing kidney disease:
- Follow instructions on medicines that you buy off the shelf. If you use an off-the-shelf pain reliever, such as ibuprofen (Advil, Motrin IB, others), it's important to follow the instructions on the package. Taking too many pain relievers for a long time could lead to kidney damage.
- Keep a healthy weight. If you're at a healthy weight, being physically active most days of the week can help keep it that way. If you need to lose weight, talk with your healthcare team about a weight-loss plan.
- Don't smoke. Cigarette smoking can hurt the kidneys and make existing kidney damage worse. If you smoke, talk to your healthcare team about ways to quit. Support groups, counseling and medicines can help you to stop.
- Manage medical conditions with the help of your healthcare team. If you have diseases or conditions that raise your risk of kidney disease, work with your healthcare team to manage them. Ask about tests to look for signs of kidney damage. If you have high blood pressure, follow a low-sodium diet, check your blood pressure regularly at home and take any medicines you've been prescribed to lower your blood pressure. This can help protect your kidneys.
Diagnosis

To diagnose chronic kidney disease, a healthcare professional needs to assess your risk of the condition. They might ask you about your symptoms, including any changes in your urinary habits. You also might be asked about your personal or family history of kidney disease. Your healthcare professional also may ask about a history of other conditions, such as diabetes, high blood pressure, and autoimmune or inherited diseases. They also typically review with you any medicines you take.
Your healthcare professional is likely to examine your body. The exam may check for problems with the heart or blood vessels. A neurological exam also is common.
For kidney disease diagnosis, you also might need certain tests and procedures. These can help show how serious your kidney disease is. Your health care professional may refer to this as staging the disease. Tests might include:
- Blood tests. Kidney function tests look for the level of waste products in your blood. Waste products include creatinine and urea.
- Urine tests. Checking a sample of your urine can reveal signs of chronic kidney disease. Urine tests also could provide clues about what's causing your kidney disease. Having protein, called albumin, and blood present in the urine could be a sign of kidney disease.
- Imaging tests. Your healthcare professional might use ultrasound to view your kidneys. Ultrasound can show the structure and size of the kidneys. Other imaging tests might be used in some cases.
-
Removing a sample of kidney tissue for testing. Your healthcare professional might recommend a kidney biopsy. A biopsy is a procedure to remove a sample of kidney tissue for testing in a lab. It uses a long, thin needle that is inserted through the skin and into a kidney. The biopsy sample is sent to a lab for testing. In the lab, tests can help reveal what's causing a kidney problem.
A kidney biopsy is usually done when the cause of kidney disease isn't clear, especially if kidney function is quickly declining and there's a lot of protein in the urine.
Results from these tests can help your healthcare team make a treatment plan.
Treatment
Depending on the cause, some types of kidney disease can be treated. Often, though, chronic kidney disease has no cure. Even in that case, treatment is still needed to preserve kidney function for as long as possible.
Treatment for chronic kidney disease usually aims to help manage symptoms, reduce complications and slow the progress of the disease. If your kidneys become badly damaged, treatment for end-stage kidney disease might be needed.
Treating the cause
Your healthcare team will work with you on ways to slow down the progress of your kidney disease and help manage what's causing it. Treatment options vary and depend on the cause. For instance, your treatment may aim to lower high blood pressure or manage diabetes. But kidney damage can continue to worsen even after an underlying condition has been controlled.
Slowing progression of kidney disease
No matter what causes kidney disease, there are certain things you can do to protect the kidneys and slow down the rate of kidney function getting worse. These include:
- A low-salt diet. People with kidney disease should avoid adding extra salt to foods and limit how much salt, also called sodium, they have each day to around 2,000 milligrams.
- Blood pressure management. High blood pressure can develop or get worse with kidney disease. Do regular checks of your blood pressure at home. Aim to keep blood pressure at 130/80 or less. Eating the right foods, getting regular exercise and blood pressure medicines can help maintain blood pressure management.
- A lower protein diet. Eating less protein can reduce how hard your kidneys need to work to get rid of the extra waste. A registered dietitian can suggest ways to lower how much protein you have while still eating a healthy diet with enough calories.
- Certain blood pressure medicines. Taking an angiotensin-converting enzyme (ACE) inhibitor or an angiotensin 2 receptor blocker (ARB) has been shown to protect the kidneys. These drugs are blood pressure medicines used in people with heart disease.
- Certain diabetes medicines. Drugs called SGLT2 inhibitors were designed for treating diabetes, but later on showed promise for protecting the kidneys and the heart. These medicines are most often helpful for people who have mild to moderate kidney disease and especially for those who have protein in their urine.
Treating complications of chronic kidney disease
Kidney disease complications can be managed to make you more comfortable. Treatments might include:
-
Lower high blood pressure. People with kidney disease can have worsening high blood pressure. Your healthcare professional might have you take medicines to lower your blood pressure. Often, people need to take more than one medicine to lower their blood pressure. This might include an ACE inhibitor or ARB, along with a diuretic. A diuretic also is called a water pill, and it helps lower blood pressure by removing extra fluid from the body.
High blood pressure medicines can at first decrease kidney function and change electrolyte levels. So, you might need frequent blood tests to check your condition.
- Lessen swelling. Chronic kidney disease is one cause of fluid buildup in the body, which can lead to leg and ankle swelling or shortness of breath. Diuretic medicines can help maintain the balance of fluids in the body and reduce swelling.
-
Treat anemia. Treatment might focus on helping the body make more red blood cells. This might lessen fatigue and weakness from anemia. Anemia happens when you don't have enough healthy red blood cells to carry oxygen to the body's tissues.
A shot containing a hormone called erythropoietin may be used to treat anemia. A condition known as iron-deficiency anemia also is common in people with kidney disease. Iron-deficiency anemia can develop after starting on the erythropoietin shots to treat anemia. When this happens, you need to take iron pills or in some cases, have an iron infusion given through a vein.
- Reduce heart disease risk. If you have high cholesterol, your healthcare professional might recommend medicines called statins. Statins can help lower cholesterol. People with chronic kidney disease often have high levels of bad cholesterol, which can raise the risk of heart disease. A healthy diet and regular exercise also are important.
- Prevent bone disease. Calcium and vitamin D supplements help prevent weak bones and lower the risk of broken bones. Your care team may recommend a low phosphorus diet. You also might take medicine known as a phosphate binder. This medicine is taken with meals and can lower the amount of phosphate in the blood and protect blood vessels from damage by calcium deposits. Calcium deposits are sometimes called calcifications.
- Treat acid buildup. If acid buildup causes a substance known as bicarbonate to drop in your blood, your healthcare professional may recommend taking sodium bicarbonate, or baking soda pills. Eating less animal protein also may help.
Your healthcare professional might recommend regular follow-up testing. Follow-up testing makes it possible to check if kidney disease is getting worse. In many cases, starting treatment earlier can help prevent severe complications.
Preparing for kidney failure
Complete or near-complete kidney failure may happen when the kidneys can't keep up with waste, fluid and salt clearance on their own. When this happens, family members of the person with kidney failure might notice that symptoms get worse. They may include:
- Poor appetite.
- Lack of energy.
- Poor sleep.
- Mental decline.
- Daily nausea.
Lab tests might show very low kidney function and high potassium in the blood. When this happens, you have end-stage kidney disease.
Treatment options for kidney failure in end-stage kidney disease include:
-
Kidney transplant. A kidney transplant is surgery to place a healthy kidney from a donor into your body. Transplanted kidneys can come from deceased or living donors. You don't need to be on dialysis to have a kidney transplant.
A kidney transplant is considered the best treatment for kidney failure, but not everyone can have a kidney transplant. Having a kidney transplant requires a full and detailed evaluation process. After a transplant, you'll need to take medicines to keep your body from rejecting the new organ. The medicines need to be taken for the rest of your life.
-
Dialysis. Dialysis artificially removes waste products and extra fluid from your blood when your kidneys can no longer do this. There are two forms of dialysis. In hemodialysis, a machine filters waste and excess fluids from your blood. Hemodialysis usually is done in a dialysis center for 3 to 4 hours three times a week. In some cases, people may qualify to do hemodialysis themselves at home.
In peritoneal dialysis, a thin tube is placed with a minor surgery into your stomach area. Clean fluid slowly fills that space and remains there. The fluid is called dialysis solution. A natural membrane in the stomach area is used as the filter. The dialysis solution absorbs waste and excess fluids. After a few hours, the dialysis solution is drained from the body, carrying the waste with it. This type of dialysis happens at home. Most people can use a machine called a cycler to do the fluid exchanges at night, while they sleep.
- Comprehensive medical management. For some who choose not to have dialysis or a kidney transplant, there is another option. You may choose care that focuses on treating symptoms and keeping you comfortable as kidney disease progresses to end of life. People with kidney failure don't survive long without dialysis or a transplant. Your care team may include an expert in palliative care, which is specialized medical care that focuses on comfort measures and quality of life in people with serious illnesses.
The kidney transplant and dialysis treatment options also are called kidney replacement therapy.
Lifestyle and home remedies
As part of the treatment for chronic kidney disease, your healthcare team might suggest that you follow a special diet. Careful choices about what to eat and drink can limit how hard the kidneys have to work.
Ask your healthcare professional for a referral to a registered dietitian. A dietitian can study your diet and suggest ways to make it easier on your kidneys.
Your personal situation, including how well your kidneys are working and your overall health, can affect what dietary changes you may need to follow. For example, you might need to:
- Avoid products with added salt. Lower the amount of sodium you eat each day by staying away from salty snack foods and other foods with added salt. These include many ready-made foods, such as frozen dinners and canned soups and vegetables. Processed meats and cheeses also tend to be high in salt.
- Choose lower potassium foods. High-potassium foods include bananas, oranges, potatoes, spinach and tomatoes. Examples of low-potassium foods include apples, cabbage, carrots, green beans, grapes and strawberries. Since many salt substitutes contain potassium, you may want to stop using them if you have kidney failure.
- Limit the amount of protein you eat. Your registered dietitian will estimate how many grams of protein you need each day. Based on that amount, your dietitian can make suggestions on what to eat. High protein foods include lean meats, eggs, milk, cheese and beans. Low protein foods include vegetables, fruits, breads and cereals.
Coping and support
Receiving a diagnosis of chronic kidney disease may worry you. And making changes to your diet can be challenging and sometimes confusing. If you're feeling overwhelmed by your diagnosis, it might help to:
- Connect with other people who have kidney disease. Someone else who's going through the same thing as you can understand what you're feeling. They also can offer unique support. Ask your healthcare professional about support groups in your area. Or contact the American Association of Kidney Patients, the National Kidney Foundation or the American Kidney Fund. These organizations can help connect you with groups in your area.
- Stick to your usual routine as much as possible. Try to keep doing the activities you enjoy. Continue working if your condition allows. This can help you cope with feelings of sadness or loss that you might have.
- Be active most days of the week. If your healthcare professional says it's OK, keep up your activity level. Aim for at least 30 minutes of physical activity most days of the week. This can help with fatigue and stress.
- Talk with someone you trust. You might have a friend or family member who is a good listener. Or you may find it helpful to talk with a faith leader or someone else you trust. Ask your healthcare professional for a referral to a social worker or counselor.
Preparing for an appointment
You may start by seeing the healthcare professional who provides your primary care. If lab tests show that you have kidney damage, you might be referred to a nephrologist. A nephrologist is a doctor who specializes in kidney conditions.
What you can do
Before your appointment, it's a good idea to:
- Be aware of any restrictions before the appointment. When you make the appointment, ask if there's anything you need to do in advance, such as change your diet, so that you're ready for any tests you may need.
- Write down any symptoms you have, including any that may seem unrelated to your kidneys or urinary function, and when they started.
- Write down key personal information, including any major stresses or recent life changes.
- Make a list of all medicines, vitamins or supplements you take and how much you take.
- Consider bringing a family member or friend along. It can be hard to remember all the information you get during an appointment. Someone who comes with you may remember things that you missed or forgot.
- Write down questions to ask your healthcare team.
For chronic kidney disease, some basic questions to ask include:
- What's the level of damage to my kidneys?
- What kinds of tests do I need?
- What's causing my condition?
- Is my kidney function getting worse?
- Can the damage to my kidneys be undone?
- What next steps do you recommend?
- Are there alternatives to the treatment you're suggesting?
- What are the possible side effects of treatment?
- I have other health conditions. How can I best treat them together?
- How often do I need to have tests to see how well my kidneys are working?
- Do I need to eat a special diet?
- Can you refer me to a dietitian who can help me plan my meals?
- Where can I find more information?
Don't hesitate to ask other questions during your appointment.
What to expect from your doctor
During your appointment, you may be asked questions, such as:
- When did you first start having symptoms?
- How have your symptoms changed over time?
- Have you been diagnosed with or treated for high blood pressure?
- Have you noticed changes in your urinary habits?
© 1998-2025 Mayo Foundation for Medical Education and Research(MFMER). All rights reserved. Terms of Use
