Ampullary cancer
Conditions
Overview
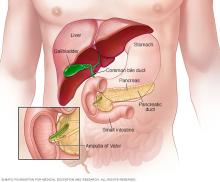
Ampullary cancer is cancer that starts as a growth of cells in the ampulla of Vater. The ampulla of Vater is located where the bile duct and pancreatic duct join and empty into the small intestine. Ampullary (AM-poo-la-ree) cancer is rare.
Ampullary cancer forms near many other parts of the digestive system. This includes the liver, pancreas and small intestine. When ampullary cancer grows, it may affect these other organs.
Ampullary cancer treatment often involves surgery to remove the cancer. Treatment also may include radiation therapy and chemotherapy to kill cancer cells.
Symptoms
Signs and symptoms of ampullary cancer may include:
- Yellowing of the skin and whites of the eyes, called jaundice.
- Diarrhea.
- Clay-colored stools.
- Abdominal pain.
- Fever.
- Blood in the stool.
- Nausea.
- Vomiting.
- Weight loss.
When to see a doctor
Make an appointment with a doctor or other healthcare professional if you have any persistent symptoms that worry you.
Causes
It's not clear what causes ampullary cancer.
Ampullary cancer happens when cells in the ampulla of Vater develop changes in their DNA. A cell's DNA holds the instructions that tell a cell what to do. In healthy cells, the DNA gives instructions to grow and multiply at a set rate. The instructions tell the cells to die at a set time. In cancer cells, the changes give different instructions. The changes tell the cancer cells to make many more cells quickly. Cancer cells can keep living when healthy cells would die. This causes too many cells.
The cancer cells might form a mass called a tumor. The tumor can grow to invade and destroy healthy body tissue. In time, cancer cells can break away and spread to other parts of the body. When cancer spreads, it's called metastatic cancer.
Risk factors
Factors that can increase the risk of ampullary cancer include:
- Increasing age. Ampullary cancer is more common in adults older than 70.
- DNA changes that run in families. Some DNA changes that are passed down from your parents can increase your risk of ampullary cancer and other cancers. Examples include the DNA changes that are linked to Lynch syndrome, familial adenomatous polyposis, also called FAP, and Peutz-Jeghers syndrome.
There is no way to prevent ampullary cancer.
Diagnosis
Tests and procedures used to diagnose ampullary cancer include:
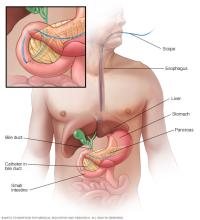
Passing a thin, flexible scope down the throat, called an endoscopy
Endoscopy is a procedure to examine the digestive system. It uses a long, thin tube with a tiny camera, called an endoscope. The endoscope passes down the throat, through the stomach and into the small intestine. It allows the healthcare team to see the ampulla of Vater.
Special tools can pass through the endoscope to collect a sample of tissue for testing.
Endoscopy also can be used to create images. For instance, endoscopic ultrasound may help capture images of ampullary cancer.
Sometimes a dye is injected into the bile duct using endoscopy. This procedure is called endoscopic retrograde cholangiopancreatography. The dye shows up on X-rays. It can help look for blockages in the bile duct or pancreatic duct.
Imaging tests
Imaging tests make pictures of the body. They can show the location and size of ampullary cancer. Imaging tests may help the healthcare team understand more about the cancer and determine whether it has spread beyond the ampulla of Vater.
Imaging tests may include:
- Endoscopic ultrasound.
- Endoscopic retrograde cholangiopancreatography.
- Magnetic resonance cholangiopancreatography.
- CT scan.
Removing a sample of tissue for testing, called biopsy
A biopsy is a procedure to remove a sample of tissue for testing in a lab. The sample is tested in a lab to see if it is cancer. Other special tests give more details about the cancer cells. Healthcare teams use this information to make a treatment plan.
Treatment
Ampullary cancer treatment often starts with surgery to remove the cancer. Other treatments may include chemotherapy and radiation. These other treatments can be done before or after surgery. The best treatment for your ampullary cancer depends on several factors. These include the size of the cancer, your overall health and your preferences.
Surgery
Surgery options may include:
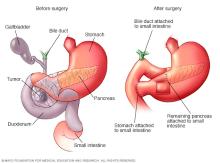
- Surgery to remove the cancer and nearby structures. The Whipple procedure, also known as a pancreaticoduodenectomy, involves removing the cancer by removing the head of the pancreas. The surgeon also removes a portion of the small intestine, gallbladder and part of the bile duct. The Whipple procedure can be done using a large incision in the abdomen. It also can be done using several small incisions.
- Surgery for very small cancers. For very small ampullary cancers and precancerous tumors, it may be possible to remove the cancer with tools passed through an endoscope. This is called an endoscopic surgery.
- Surgery to place a stent. Sometimes the goal of surgery is to make you more comfortable. If you have jaundice, surgery may be used to place a small wire mesh tube, called a stent, in your bile ducts. This tube helps drain the fluid that causes a yellowing of the skin and eyes.
Other treatments
Other treatments may be used, including:
-
Combined chemotherapy and radiation. Chemotherapy treats cancer with strong medicines. Radiation therapy treats cancer with powerful energy beams. The energy can come from X-rays, protons or other sources. Used together, these treatments may be more effective for ampullary cancers.
Combined chemotherapy and radiation may be used before surgery, to make it more likely that a cancer can be removed completely during an operation. The combined treatment also can be used after surgery to kill any cancer cells that might remain.
- Chemotherapy alone. Chemotherapy is sometimes used after surgery to kill cancer cells that might remain. In people with advanced ampullary cancer, chemotherapy may be used alone to slow the growth of the cancer.
- Targeted therapy. Targeted therapy uses medicines that attack specific chemicals in the cancer cells. By blocking these chemicals, targeted treatments can cause cancer cells to die. Targeted therapy is used to treat ampullary cancer that spreads to other parts of the body or comes back after treatment. It's only used in certain situations.
- Immunotherapy. Immunotherapy is a treatment with medicine that helps the immune system kill cancer cells. The immune system fights off diseases by attacking germs and other cells that shouldn't be in the body. Cancer cells survive by hiding from the immune system. Immunotherapy helps the immune system cells find and kill the cancer cells. It may be an option for treating ampullary cancer that spreads to other parts of the body or comes back after treatment. Immunotherapy is only used in certain situations.
Palliative care
Palliative care is a special type of healthcare that helps you feel better when you have a serious illness. If you have cancer, palliative care can help relieve pain and other symptoms. A healthcare team that may include doctors, nurses and other specially trained health professionals provides palliative care. The care team's goal is to improve quality of life for you and your family.
Palliative care specialists work with you, your family and your care team. They provide an extra layer of support while you have cancer treatment. You can have palliative care at the same time you're getting strong cancer treatments, such as surgery, chemotherapy or radiation therapy.
The use of palliative care with other treatments can help people with cancer feel better and live longer.
Coping and support
With time, you'll find what helps you cope with the uncertainty and distress of a cancer diagnosis. Until then, you may find it helps to:
- Learn enough about ampullary cancer to make decisions about your care. Ask your healthcare team about your cancer, including your test results, treatment options and, if you like, your prognosis. As you learn more about ampullary cancer, you may become more confident in making treatment decisions.
- Keep friends and family close. Keeping your close relationships strong will help you deal with your ampullary cancer. Friends and family can provide the practical support you'll need, such as helping take care of your home if you're in the hospital. And they can serve as emotional support when you feel overwhelmed by having cancer.
-
Find someone to talk with. Find someone who is willing to listen to you talk about your hopes and fears. This may be a friend or family member. The concern and understanding of a counselor, medical social worker, clergy member or cancer support group also may be helpful.
Ask your healthcare team about support groups in your area. Other sources of information include the National Cancer Institute and the American Cancer Society.
Preparing for an appointment
Make an appointment with a doctor or other healthcare professional if you have any symptoms that worry you.
If your healthcare professional thinks you might have ampullary cancer, you may be referred to a specialist. This might be a doctor who specializes in treating diseases and conditions of the digestive system, called a gastroenterologist. If a cancer diagnosis is made, you also may be referred to a doctor who specializes in treating cancer. This doctor is called an oncologist.
Because appointments can be brief, it's a good idea to be prepared. Here's some information to help you get ready.
What you can do
- Be aware of any pre-appointment restrictions. At the time you make the appointment, be sure to ask if there's anything you need to do in advance, such as restrict your diet.
- Write down symptoms you're experiencing, including any that may not seem related to the reason for which you scheduled the appointment.
- Write down key personal information, including major stresses or recent life changes.
- Make a list of all medicines, vitamins or supplements you're taking and the doses.
- Take a family member or friend along. Sometimes it can be difficult to remember all the information provided during an appointment. Someone who accompanies you may remember something that you missed or forgot.
- Write down questions to ask your healthcare team.
Your time with your healthcare team is limited, so preparing a list of questions can help you make the most of your time together. List your questions from most important to least important in case time runs out. For ampullary cancer, some basic questions to ask include:
- What's likely causing my symptoms?
- Other than the most likely cause, what are other possible causes for my symptoms?
- What tests do I need?
- What's the best course of action?
- What are the alternatives to the primary approach you're suggesting?
- I have other health conditions. How can I best manage them together?
- Are there restrictions I need to follow?
- Should I see a specialist?
- Are there brochures or other printed material I can have? What websites do you recommend?
Don't hesitate to ask other questions.
What to expect from your doctor
Be prepared to answer questions, such as:
- When did your symptoms begin?
- Have your symptoms been continuous or occasional?
- How severe are your symptoms?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
© 1998-2026 Mayo Foundation for Medical Education and Research(MFMER). All rights reserved. Terms of Use
