Fecal incontinence
Conditions
Overview
Fecal incontinence is accidental passing of solid or liquid stool. Fecal incontinence may happen when a person has a sudden urge to pass stool and cannot get to a toilet in time. Also, stool may leak when a person doesn't sense the need to pass stool.
Common causes of fecal incontinence include diarrhea, constipation, and muscle or nerve damage. Fecal incontinence can affect a person's ability to work, socialize or do typical daily activities. It often causes embarrassment or emotional stress.
Diagnosis and treatment are often avoided because the condition is difficult to discuss with a healthcare professional. Treatments can improve fecal incontinence and overall quality of life.
Fecal incontinence also may be called bowel incontinence or accidental bowel leakage.
Symptoms
The main symptom is not being able to control passing stool. This may happen during a short-term illness that causes diarrhea. For some people, fecal incontinence is an ongoing condition.
There are two types of fecal incontinence:
- Urge incontinence is the sudden urge to pass stool but not being able to control the urge. The need to pass stool may come on so suddenly that it's not possible to get to the toilet in time.
- Passive incontinence is passing stool when a person isn't aware of the need to pass stool. A person may not be able to feel that the rectum is full of stool.
Fecal incontinence also may be leakage of stool when a person passes gas.
When to see a doctor
See your healthcare professional if you or your child develops fecal incontinence. This is especially important if fecal incontinence:
- Happens often.
- Causes emotional distress.
- Affects your ability to do daily activities.
- Causes you to avoid time with family and friends.
Often, people are embarrassed to talk about fecal incontinence. But the sooner you're evaluated, the sooner you may find some relief from your symptoms.
Causes
For many people, there is more than one cause of fecal incontinence.
Causes may include:
Diarrhea and constipation. Very soft and very hard stools can lead to fecal incontinence. Problems include:
- Loose or watery stool that quickly fills the rectum and is difficult to hold.
- Large, hard stool that blocks the rectum and results in leakage of softer stool around it.
Damaged or weakened muscles. The muscles of the anus, rectum and pelvic floor control the holding and passing of stool. Damaged or weak muscles can cause fecal incontinence. Conditions that can weaken or damage muscles include:
- Injury during vaginal delivery, particularly with forceps.
- Surgical cut of the vagina during delivery, called an episiotomy.
- Injury from accidents, surgery or radiation therapy.
- Age-related weakening of muscles.
Nervous system disorders. Injury or illness can affect how the nerves and muscles of the anus, rectum or pelvis work. Nervous system disorders also may affect a person's awareness of the need for passing stool. These conditions may include:
- Diseases of the brain, such Parkinson's disease, Alzheimer's disease or other dementias, stroke, or cerebral palsy.
- Long-term diseases affecting nerve function, such as diabetes or multiple sclerosis.
- Spinal cord injury or tumor.
- Damage to nerves during surgery.
Physical problems of the anus or rectum. Irregular physical changes in the anus or rectum can contribute to fecal incontinence. These include:
- Scarring or inflammation of the rectum — from injury or long-term disease — that affects the ability of the rectum to hold stool.
- Dropping of the rectum through the anus, called rectal prolapse.
- Hemorrhoids that may prevent the closing of the anal muscles.
- Bulging of the rectum into the vagina, also called rectocele.
Risk factors
A number of factors may increase your risk of developing fecal incontinence, including:
- Age. Fecal incontinence is more likely in adults over 65.
- Sex. Fecal incontinence is more common in women, likely because of possible injuries during delivery. Hormone treatments for menopause also may increase the risk.
- Diseases of the digestive system. The risk of fecal incontinence is increased with long-term diseases that affect the intestines. These include:
- Inflammatory bowel disease, such as Crohn's disease.
- Irritable bowel syndrome.
- Celiac disease.
- Mental disability. A mental disability or dementia may affect a person's ability to plan to use the toilet or be aware of the need to use the toilet.
- Physical disability. A physical disability or limited mobility may make it difficult to reach a toilet in time. An injury that caused a physical disability may cause nerve or muscle damage that increases the risk of fecal incontinence.
- Lifestyle factors. Lifestyle factors that increase the risk of incontinence include being overweight, not being active, smoking, and drinking caffeinated and alcoholic beverages.
Complications
Complications of fecal incontinence may include:
- Emotional distress. Many people feel embarrassed about fecal incontinence. And they often experience anxiety or depression. They may try to hide the problem and avoid social situations.
- Tissue irritation. The skin around the anus is delicate and sensitive. Repeated contact with stool can lead to pain and itching. Sores, called ulcers, may appear in the tissues of the rectum.
Prevention
Depending on the cause, it may be possible to improve or prevent fecal incontinence. These actions may help:
- Reduce constipation. Increase your exercise, eat more high-fiber foods and drink plenty of fluids.
- Control diarrhea. Avoid food or drinks that may make diarrhea worse, such as caffeinated drinks, alcohol, dairy products and fatty foods.
- Do not strain. Straining during bowel movements can eventually weaken anal sphincter muscles or damage nerves.
Diagnosis
Your healthcare professional will ask questions about your symptoms, diet and medical history. A detailed medical exam will include:
- Anal and rectal exam. Your healthcare professional will look at and examine the area around the anus to look for reflexes of the anal muscles and look for signs of irregular tissues. An exam with a gloved finger inserted in the anus can detect problems with muscles or other tissues of the rectum. The presence of large, hard stool also can be detected.
- Neurological exam. This exam tests the general health of the nervous system, such as sensation, reflexes, coordination and balance.
Tests of rectal and anal function
Tests to see how well you are able to pass stool include:
- Anorectal manometry. A narrow, flexible device is inserted into the anus and rectum. The test provides information about how well the muscles and nerves of the anus and rectum work. It also measures how much the rectum can expand.
- Balloon expulsion test. A small balloon is inserted into the rectum and filled with water. You'll then be asked to go to the toilet to expel the balloon. This test shows how well you can empty stool from the rectum.
Imaging tests
Tests for visualizing the rectum and colon include:
- Endoscopy. A flexible tube with a camera is used to exam the rectum and colon. Variations of this test may be used to see only the rectum, the lower part of the colon or the entire colon. An endoscopy can show signs of inflammation, cancer or other irregular tissues.
- Endoscopic ultrasound. This device combines endoscopy and ultrasound images to examine tissues of the rectum and colon.
- Defecography. This test may be done with X-ray imaging or magnetic resonance imaging (MRI). The test is done with special equipment that allows imaging while you are passing stool. This provides information about both the physical condition and function of the rectum and anus.
- Anorectal MRI. An MRI also can provide information about the condition of muscles of the anus and rectum.
Treatment
The goals of therapy are to manage conditions that cause or worsen fecal incontinence and to improve the function of the rectum and anus.
Diet and lifestyle changes
The first step is making changes to diet and lifestyle habits. These may include:
Adding more high-fiber foods gradually, such as:
- Vegetables and most fruits.
- Whole-grain foods.
- Beans and other legumes.
Avoiding foods that can cause diarrhea. These include:
- Drinks with caffeine, alcohol or artificial sweeteners.
- Fatty foods and dairy products.
- Foods with added fructose or naturally high fructose, such as apples, peaches and pears.
- Spicy foods.
Making other healthy changes in behavior such as:
- Exercising regularly.
- Drinking plenty of water.
- Losing or managing weight.
- Quitting smoking.
Medicines
Your healthcare professional may recommend medicines or supplements to treat conditions related to fecal incontinence. These include:
- Anti-diarrheal drugs such as loperamide (Imodium A-D), diphenoxylate and atropine (Lomotil), and bismuth subsalicylate (Pepto-Bismal, Kaopectate, others).
- Fiber supplements such as methylcellulose (Citrucel) and psyllium (Metamucil, Konsyl, others), if chronic constipation is causing your incontinence.
- Laxatives that help with passing stool include magnesium hydroxide (Phillips' Milk of Magnesia, Dulcolax Liquid, others), polyethylene glycol (MiraLAX) and bisacodyl (Correctol, Dulcolax Laxative, others).
Exercise and training
Exercises help strengthen the muscles of the anus, rectum and pelvic floor. These exercises can improve your control over when you pass stool. Options include:
- Kegel exercises. These exercises strengthen the muscles of the anus and pelvic floor muscles. Contract the muscles that you use to stop passing gas or urinating. Hold the contraction for three seconds, then relax for three seconds. Repeat this pattern 10 to 15 times. As your muscles strengthen, hold the contraction longer. Gradually work your way up to three sets of 10 to 15 contractions every day.
- Biofeedback training. Specially trained physical therapists provide exercises and information. Monitoring devices provide feedback that you can see or hear to help you understand the sensations and muscle activity needed to control passing stool. Biofeedback training can help you:
- Strengthen anal and pelvic floor muscles.
- Sense when stool is ready to be released.
- Contract muscles when you need to delay passing stool.
- Bowel training. Your doctor may recommend passing stool at a specific time of day, such as after a meal. Following a schedule for using the toilet can help you gain greater control.
Other treatments
Other treatments may be used when more conservative treatments don't work. These include:
- Bulking agents. Injections of nonabsorbable bulking agents can thicken the walls of the anus. This helps prevent leakage.
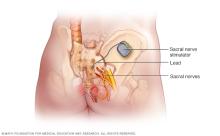
- Sacral nerve stimulation. The sacral nerves run from your spinal cord to muscles in the pelvis. They regulate the sensation and strength of your rectal and anal sphincter muscles. Implanting a device that sends small electrical impulses to the nerves can improve how these muscles work.
- Inserted devices. An anal plug is a disposable device that is used to block leakage. A vaginal insert is an inflatable balloon that puts pressure on the lower part of the rectum to prevent leakage.
Surgery
Surgery may be necessary to correct an underlying problem, such as rectal prolapse, that causes fecal incontinence. Surgery also is used when other treatments are not working. The options include:
- Surgery for underlying problems. Surgeries can repair tissue that cause or contribute to fecal incontinence. These include rectal prolapse, a rectocele or hemorrhoids. These surgeries may be needed in order for lifestyle treatments and medicines to work.
- Sphincteroplasty. This procedure repairs a damaged or weakened anal sphincter that occurred during childbirth. Doctors identify an injured area of muscle and free its edges from the surrounding tissue. They then bring the muscle edges back together and sew them in an overlapping fashion. This helps strengthen the muscle and tighten the sphincter. The procedure doesn't always work, and the benefit decreases over time.
- Colostomy, also called bowel diversion. This surgery diverts stool through an opening in the abdomen. Doctors attach a special bag to this opening to collect the stool. Colostomy is used after other treatments haven't been successful.
Lifestyle and home remedies
Diaries
Keeping diaries for a few weeks can help you manage symptoms and communicate with your healthcare professional. Consider the following:
- Food diary. Write down what you have for meals, snacks and drinks. You may discover a pattern between certain foods and fecal incontinence. Once you've identified problem foods, stop eating them and see if your incontinence improves.
- Stool diary. Write down when you pass stool and when you experience incontinence. Also, write down what the stool is like. Your healthcare professional can provide you with a picture chart to help you describe stool.
Skin care
You can help avoid further discomfort from fecal incontinence by keeping the skin around your anus as clean and dry as possible. To relieve anal discomfort and get rid of odor related to fecal incontinence:
- Use unscented wipes. Use scent-free, alcohol-free wipes instead of dry toilet paper after passing stool.
- Wash with water. Gently wash the area around the anus with water and scent-free soap after passing stool or an incontinence episode. Showering or soaking in a bath also may help.
- Dry thoroughly. Allow the area to air-dry, if possible. If you're short on time, you can gently pat the area dry with toilet paper or a clean washcloth.
- Apply a cream or powder. Moisture-barrier creams help keep irritated skin from having direct contact with feces. Be sure the area is clean and dry before you apply any cream. Nonmedicated talcum powder or cornstarch also may help relieve anal discomfort.
- Wear cotton underwear and loose clothing. Tight clothing can restrict airflow, making skin problems worse. Change soiled underwear quickly.
When medical treatments can't completely eliminate incontinence, products such as absorbent pads and disposable underwear can help you manage the problem. If you use pads or adult diapers, be sure they have an absorbent wicking layer on top. This helps keep moisture away from your skin.
Coping and support
For some people, including children, fecal incontinence is a relatively minor problem. It's typically limited to occasional soiling of their underwear. For others, the condition can be a more challenging, ongoing condition.
If you have fecal incontinence
You may feel reluctant to leave your house because you're concerned about making it to a toilet in time. Try these practical tips:
- Use the toilet right before you go out.
- If you expect that you'll be incontinent, wear a pad or a disposable undergarment.
- Carry supplies for cleaning up and a change of clothing with you.
- Know where toilets are located before you need them. This can help you get to them quickly.
- Use nonprescription pills to reduce the smell of stool and gas. These are known as fecal deodorants.
Because fecal incontinence can be distressing, it's important to take steps to deal with it. Treatment can help improve your quality of life and raise your self-esteem.
Preparing for an appointment
You may start by seeing your primary healthcare professional. You may then be referred to a provider who specializes in treating digestive conditions, called a gastroenterologist.
Here's some information to help you get ready for your appointment.
What you can do
When you make the appointment, ask if there's anything you need to do in advance, such as fasting before having a specific test. Make a list of:
- Your symptoms, including any that seem unrelated to the reason for your appointment.
- Key personal information, including major stresses, recent life changes and family medical history.
- All medicines, vitamins or other supplements you take, including the doses.
- Bring a family member or friend with you if possible, to help you remember the information you're given.
- Make a list of questions to ask during the appointment.
For fecal incontinence, some basic questions to ask include:
- What's likely causing my symptoms?
- Other than the most likely cause, what are other possible causes for my symptoms?
- What tests do I need?
- Is my condition likely temporary or chronic?
- What's the best course of action?
- What are the alternatives to the primary approach you're suggesting?
- I have other health conditions. Will treatment for fecal incontinence complicate my care for these conditions?
- Are there restrictions I need to follow?
- Should I see a specialist?
- Are there brochures or other printed material I can have? What websites do you recommend?
What to expect from your doctor
Your provider is likely to ask you several questions, such as:
- When did your symptoms begin?
- Have your symptoms been continuous or do they come and go?
- How severe are your symptoms?
- Does anything seem to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
- Do you avoid any activities because of your symptoms?
- Do you have other conditions such as diabetes, multiple sclerosis or frequent constipation?
- Do you have diarrhea?
- Have you ever been diagnosed with a disorder of the colon?
- Have you ever had radiation therapy to your pelvic area?
- Were forceps used or did you have an episiotomy during childbirth?
- Do you also have urinary incontinence?
What you can do in the meantime
Do not eat foods or do activities that worsen your symptoms. This might include avoiding caffeine, fatty or greasy foods, dairy products, spicy foods, or anything that makes your incontinence worse.
© 1998-2026 Mayo Foundation for Medical Education and Research(MFMER). All rights reserved. Terms of Use
