Gallstones
Conditions
Overview
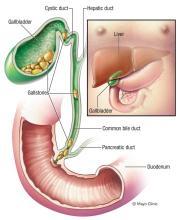
Gallstones are hardened deposits of digestive fluid that can form in your gallbladder. Your gallbladder is a small, pear-shaped organ on the right side of your abdomen, just beneath your liver. The gallbladder holds a digestive fluid called bile that's released into your small intestine.
Gallstones range in size from as small as a grain of sand to as large as a golf ball. Some people develop just one gallstone, while others develop many gallstones at the same time.
People who experience symptoms from their gallstones usually require gallbladder removal surgery. Gallstones that don't cause any signs and symptoms typically don't need treatment.
Symptoms
Gallstones may cause no signs or symptoms. If a gallstone lodges in a duct and causes a blockage, the resulting signs and symptoms may include:
- Sudden and rapidly intensifying pain in the upper right portion of your abdomen
- Sudden and rapidly intensifying pain in the center of your abdomen, just below your breastbone
- Back pain between your shoulder blades
- Pain in your right shoulder
- Nausea or vomiting
Gallstone pain may last several minutes to a few hours.
When to see a doctor
Make an appointment with your doctor if you have any signs or symptoms that worry you.
Seek immediate care if you develop signs and symptoms of a serious gallstone complication, such as:
- Abdominal pain so intense that you can't sit still or find a comfortable position
- Yellowing of your skin and the whites of your eyes (jaundice)
- High fever with chills
Causes
It's not clear what causes gallstones to form. Doctors think gallstones may result when:
- Your bile contains too much cholesterol. Normally, your bile contains enough chemicals to dissolve the cholesterol excreted by your liver. But if your liver excretes more cholesterol than your bile can dissolve, the excess cholesterol may form into crystals and eventually into stones.
- Your bile contains too much bilirubin. Bilirubin is a chemical that's produced when your body breaks down red blood cells. Certain conditions cause your liver to make too much bilirubin, including liver cirrhosis, biliary tract infections and certain blood disorders. The excess bilirubin contributes to gallstone formation.
- Your gallbladder doesn't empty correctly. If your gallbladder doesn't empty completely or often enough, bile may become very concentrated, contributing to the formation of gallstones.
Types of gallstones
Types of gallstones that can form in the gallbladder include:
- Cholesterol gallstones. The most common type of gallstone, called a cholesterol gallstone, often appears yellow in color. These gallstones are composed mainly of undissolved cholesterol, but may contain other components.
- Pigment gallstones. These dark brown or black stones form when your bile contains too much bilirubin.
Risk factors
Factors that may increase your risk of gallstones include:
- Being female
- Being age 40 or older
- Being a Native American
- Being a Hispanic of Mexican origin
- Being overweight or obese
- Being sedentary
- Being pregnant
- Eating a high-fat diet
- Eating a high-cholesterol diet
- Eating a low-fiber diet
- Having a family history of gallstones
- Having diabetes
- Having certain blood disorders, such as sickle cell anemia or leukemia
- Losing weight very quickly
- Taking medications that contain estrogen, such as oral contraceptives or hormone therapy drugs
- Having liver disease
Complications
Complications of gallstones may include:
- Inflammation of the gallbladder. A gallstone that becomes lodged in the neck of the gallbladder can cause inflammation of the gallbladder (cholecystitis). Cholecystitis can cause severe pain and fever.
- Blockage of the common bile duct. Gallstones can block the tubes (ducts) through which bile flows from your gallbladder or liver to your small intestine. Severe pain, jaundice and bile duct infection can result.
-
Blockage of the pancreatic duct. The pancreatic duct is a tube that runs from the pancreas and connects to the common bile duct just before entering the duodenum. Pancreatic juices, which aid in digestion, flow through the pancreatic duct.
A gallstone can cause a blockage in the pancreatic duct, which can lead to inflammation of the pancreas (pancreatitis). Pancreatitis causes intense, constant abdominal pain and usually requires hospitalization.
- Gallbladder cancer. People with a history of gallstones have an increased risk of gallbladder cancer. But gallbladder cancer is very rare, so even though the risk of cancer is elevated, the likelihood of gallbladder cancer is still very small.
Prevention
You can reduce your risk of gallstones if you:
- Don't skip meals. Try to stick to your usual mealtimes each day. Skipping meals or fasting can increase the risk of gallstones.
- Lose weight slowly. If you need to lose weight, go slow. Rapid weight loss can increase the risk of gallstones. Aim to lose 1 or 2 pounds (about 0.5 to 1 kilogram) a week.
- Eat more high-fiber foods. Include more fiber-rich foods in your diet, such as fruits, vegetables and whole grains.
- Maintain a healthy weight. Obesity and being overweight increase the risk of gallstones. Work to achieve a healthy weight by reducing the number of calories you eat and increasing the amount of physical activity you get. Once you achieve a healthy weight, work to maintain that weight by continuing your healthy diet and continuing to exercise.
Diagnosis
Tests and procedures used to diagnose gallstones and complications of gallstones include:
- Abdominal ultrasound. This test is the one most commonly used to look for signs of gallstones. Abdominal ultrasound involves moving a device (transducer) back and forth across your stomach area. The transducer sends signals to a computer, which creates images that show the structures in your abdomen.
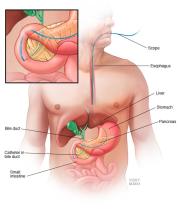
- Endoscopic ultrasound (EUS). This procedure can help identify smaller stones that may be missed on an abdominal ultrasound. During EUS your doctor passes a thin, flexible tube (endoscope) through your mouth and through your digestive tract. A small ultrasound device (transducer) in the tube produces sound waves that create a precise image of surrounding tissue.
- Other imaging tests. Additional tests may include oral cholecystography, a hepatobiliary iminodiacetic acid (HIDA) scan, computerized tomography (CT), magnetic resonance cholangiopancreatography (MRCP) or endoscopic retrograde cholangiopancreatography (ERCP). Gallstones discovered using ERCP can be removed during the procedure.
- Blood tests. Blood tests may reveal infection, jaundice, pancreatitis or other complications caused by gallstones.
Treatment
Most people with gallstones that don't cause symptoms will never need treatment. Your doctor will determine if treatment for gallstones is indicated based on your symptoms and the results of diagnostic testing.
Your doctor may recommend that you be alert for symptoms of gallstone complications, such as intensifying pain in your upper right abdomen. If gallstone signs and symptoms occur in the future, you can have treatment.
Treatment options for gallstones include:
-
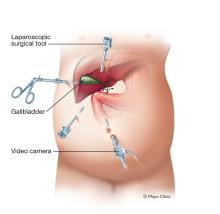
Surgery to remove the gallbladder (cholecystectomy). Your doctor may recommend surgery to remove your gallbladder, since gallstones frequently recur. Once your gallbladder is removed, bile flows directly from your liver into your small intestine, rather than being stored in your gallbladder.
You don't need your gallbladder to live, and gallbladder removal doesn't affect your ability to digest food, but it can cause diarrhea, which is usually temporary.
-
Medications to dissolve gallstones. Medications you take by mouth may help dissolve gallstones. But it may take months or years of treatment to dissolve your gallstones in this way, and gallstones will likely form again if treatment is stopped.
Sometimes medications don't work. Medications for gallstones aren't commonly used and are reserved for people who can't undergo surgery.
Preparing for your appointment
Start by seeing your family doctor or a general practitioner if you have signs or symptoms that worry you. If your doctor suspects you may have gallstones, you may be referred to a doctor who specializes in the digestive system (gastroenterologist) or to an abdominal surgeon.
Because appointments can be brief, and because there's often a lot of information to cover, it's a good idea to be well prepared. Here's some information to help you get ready, and what to expect from your doctor.
What you can do
- Be aware of any pre-appointment restrictions. At the time you make the appointment, be sure to ask if there's anything you need to do in advance, such as restrict your diet.
- Write down any symptoms you're experiencing, including any that may seem unrelated to the reason for which you scheduled the appointment.
- Write down key personal information, including any major stresses or recent life changes.
- Make a list of all medications, vitamins or supplements that you're taking.
- Take a family member or friend along. Sometimes it can be difficult to understand all the information provided during an appointment. Someone who accompanies you may remember something that you missed or forgot.
- Write down questions to ask your doctor.
Your time with your doctor is limited, so preparing a list of questions will help you make the most of your appointment. For gallstones, some basic questions to ask your doctor include:
- Are gallstones the likely cause of my abdominal pain?
- Is there a chance that my symptoms are due to something other than gallstones?
- What kinds of tests do I need?
- Is there a chance that my gallstones will go away without treatment?
- Do I need gallbladder removal surgery?
- What are the risks of surgery?
- How long does it take to recover from gallbladder surgery?
- Are there other treatment options for gallstones?
- Should I see a specialist? What will that cost, and will my insurance cover it?
- I have these other health conditions. How can I best manage them together?
- Are there brochures or other printed material that I can take with me? What websites do you recommend?
What to expect from your doctor
Your doctor may ask:
- When did you first begin experiencing symptoms?
- Are your symptoms related to eating?
- Have your symptoms ever included a fever?
- Have your symptoms been continuous or occasional?
- How severe are your symptoms?
- How long do your symptoms last?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
© 1998-2026 Mayo Foundation for Medical Education and Research(MFMER). All rights reserved. Terms of Use
