Gonorrhea
Conditions
Overview
Gonorrhea is a sexually transmitted infection, also called a sexually transmitted disease, caused by bacteria. Sexually transmitted diseases are infections spread mainly by contact with genitals or bodily fluids. Also called STDs, STIs or venereal disease, sexually transmitted infections are caused by bacteria, viruses or parasites.
Gonorrhea bacteria can infect the urethra, rectum, female reproductive tract, mouth, throat or eyes. Gonorrhea is most commonly spread during vaginal, oral or anal sexual activity. But babies can get the infection during childbirth. In babies, gonorrhea most commonly affects the eyes.
Avoiding sexual activity and not having sex prevents the spread of gonorrhea. Using a condom during sexual activity can help prevent the spread of gonorrhea. Being in a mutually monogamous relationship, in which both partners have sex only with each other and neither partner is infected, also limits the risk of an infection.
Symptoms
In many people, gonorrhea infection causes no symptoms. If there are symptoms, they often affect the genital tract, but also may occur in other places.
Gonorrhea affecting the genital tract
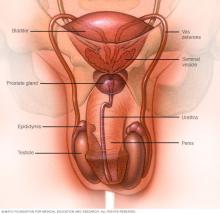
Male symptoms of gonorrhea infection include:
- Painful urination.
- Pus-like discharge from the tip of the penis.
- Pain or swelling in one testicle.
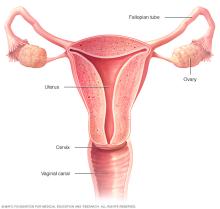
Female symptoms of gonorrhea infection include:
- Increased vaginal discharge.
- Painful urination.
- Vaginal bleeding between periods, such as after vaginal intercourse.
- Abdominal or pelvic pain.
Gonorrhea at other sites in the body
Gonorrhea also can affect these parts of the body:
- Rectum. Symptoms include anal itching, pus-like discharge from the rectum, spots of bright red blood on toilet tissue and having to strain during bowel movements.
- Eyes. Gonorrhea that affects the eyes can cause eye pain, sensitivity to light, and pus-like discharge from one or both eyes.
- Throat. Symptoms of a throat infection might include a sore throat and swollen lymph nodes in the neck.
- Joints. If one or more joints become infected by the affected joints might be warm, red, swollen and extremely painful, especially during movement. This condition is known as septic arthritis.
When to see your doctor
Make an appointment with your healthcare professional if you notice symptoms such as a burning sensation when you urinate or a pus-like discharge from your penis, vagina or rectum.
Also make an appointment if your partner has been diagnosed with gonorrhea. You might not have symptoms, but if you have the infection, you can reinfect your partner even after your partner has been treated for gonorrhea.
Causes
Gonorrhea is caused by the bacterium Neisseria gonorrhoeae. The gonorrhea bacteria are most often passed from one person to another during sexual contact, including oral, anal or vaginal intercourse.
Risk factors
Sexually active women younger than 25 and men who have sex with men are at increased risk of getting gonorrhea.
Other factors that can increase your risk include:
- Having a new sex partner.
- Having a sex partner who has other partners.
- Having more than one sex partner.
- Having had gonorrhea or another sexually transmitted infection.
Complications
Untreated gonorrhea can lead to major complications, such as:
- Infertility in women. Gonorrhea can spread into the uterus and fallopian tubes, causing pelvic inflammatory disease (PID). PID can result in scarring of the tubes, greater risk of pregnancy complications and infertility. PID requires immediate treatment.
- Infertility in men. Gonorrhea can cause inflammation in epididymis, the coiled tube above and behind the testicles that stores and transports sperm. This inflammation is known as epididymitis and without treatment it can lead to infertility.
- Infection that spreads to the joints and other areas of the body. The bacterium that causes gonorrhea can spread through the bloodstream and infect other parts of the body, including joints. Fever, rash, skin sores, joint pain, swelling and stiffness are possible results.
- Increased risk of HIV/AIDS. Having gonorrhea makes you more susceptible to infection with human immunodeficiency virus (HIV), the virus that leads to AIDS. People who have both gonorrhea and HIV can pass both diseases more readily to their partners.
- Complications in babies. Babies who get gonorrhea during birth can develop blindness, sores on the scalp and infections.
Prevention
To lower your risk of getting gonorrhea:
- Use a condom if you have sex. Not having sex and avoiding sexual activity is the surest way to prevent gonorrhea. But if you choose to have sex, use a condom during any type of sexual contact, including anal sex, oral sex or vaginal sex.
- Limit your number of sex partners. Being in a monogamous relationship in which neither partner has sex with anyone else can lower your risk.
- Be sure you and your partner are tested for sexually transmitted infections. Before you have sex, get tested and share the results with each other.
- Don't have sex with someone who appears to have a sexually transmitted infection. If someone has symptoms of a sexually transmitted infection, such as burning during urination or a genital rash or sore, don't have sex with that person.
- Consider regular gonorrhea screening. Annual screening is recommended for sexually active women younger than 25 and for older women at increased risk of infection. This includes women who have new sex partners, more than one sex partner, sex partners with other partners, or sex partners who have sexually transmitted infections.
Regular screening also is recommended for men who have sex with men. Their partners also should be tested.
A medicine called doxycycline may be an option to prevent infection among people at higher risk than average of getting gonorrhea. Higher risk groups include men who have sex with men and transgender women.
Taking doxycycline within 3 days of sexual activity lowers the risk of an infection with the bacteria that cause gonorrhea. Your healthcare professional can prescribe doxycycline and any testing you need while taking the medicine.
If you've been diagnosed with gonorrhea, do not have sex until after you and your sex partner have completed treatment and after symptoms are gone. This helps avoid getting gonorrhea again.
Diagnosis
You may be able to use a test that's available without a prescription, sometimes called an at-home test, to see if you have gonorrhea. If that test shows you have gonorrhea, you'll need to see a healthcare professional to confirm the diagnosis and start treatment.
To determine whether you have gonorrhea, your healthcare professional will analyze a sample of cells. Samples can be collected with:
- A urine test. This can help identify bacteria in your urethra.
- A swab of the affected area. A swab of your throat, urethra, vagina or rectum can collect bacteria that can be identified in a lab.
Testing for other sexually transmitted infections
Your healthcare professional may recommend tests for other sexually transmitted infections. Gonorrhea increases your risk of these infections, particularly chlamydia, which often accompanies gonorrhea.
Testing for HIV also is recommended for anyone diagnosed with a sexually transmitted infection. Depending on your risk factors, tests for other sexually transmitted infections could be beneficial as well.
Treatment
Gonorrhea treatment in adults
Adults with gonorrhea are treated with antibiotics. Due to emerging strains of drug-resistant Neisseria gonorrhoeae, the bacterium that causes gonorrhea, the Centers for Disease Control and Prevention recommends that uncomplicated gonorrhea be treated with the antibiotic ceftriaxone. This antibiotic is given as a shot, also called an injection.
After getting the antibiotic, you can still spread the infection to others for up to seven days. So avoid sexual activity for at least seven days.
Three months after treatment, the CDC also recommends getting tested for gonorrhea again. This is to make sure people haven't been reinfected with the bacteria, which can happen if sex partners aren't treated, or new sex partners have the bacteria.
Gonorrhea treatment for partners
Your sexual partner or partners from the last 60 days also need to be screened and treated, even if they have no symptoms. If you are treated for gonorrhea and your sexual partners aren't treated, you can become infected again through sexual contact. Make sure to wait until seven days after a partner is treated before having any sexual contact.
Gonorrhea treatment for babies
Babies who develop gonorrhea after being born to someone with the infection can be treated with antibiotics.
Preparing for an appointment
You'll likely see your primary healthcare professional. Here's some information to help you get ready for your appointment.
What you can do
When you make the appointment, ask if there's anything you need to do in advance, such as restrict your diet.
Make a list of:
- Your symptoms, if you have any, including those that may seem unrelated to the reason for which you scheduled the appointment, and when they began.
- All medicine, vitamins or other supplements you take, including doses.
- Questions to ask your healthcare professional.
For gonorrhea, questions to ask include:
- What tests do I need?
- Should I be tested for other sexually transmitted infections?
- Should my partner be tested for gonorrhea?
- How long should I wait before resuming sexual activity?
- How can I prevent gonorrhea in the future?
- What gonorrhea complications should I be alert for?
- Are there brochures or other printed material that I can have? What websites do you recommend?
- Will I need a follow-up visit?
Don't hesitate to ask other questions.
What to expect from your doctor
Questions your healthcare professional is likely to ask you include:
- Have your symptoms been continuous or occasional?
- How severe are your symptoms?
- Have you been exposed to sexually transmitted infections?
What you can do in the meantime
Avoid sexual activity until you see your healthcare professional. Alert your sex partners that you're having symptoms so that they can arrange to see a member of their healthcare teams for testing.
© 1998-2026 Mayo Foundation for Medical Education and Research(MFMER). All rights reserved. Terms of Use
