Left ventricular hypertrophy
Conditions
Overview
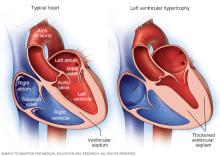
Left ventricular hypertrophy is thickening of the walls of the lower left heart chamber. The lower left heart chamber is called the left ventricle. The left ventricle is the heart's main pumping chamber.
During left ventricular hypertrophy, the thickened heart wall can become stiff. Blood pressure in the heart increases. The changes make it harder for the heart to effectively pump blood. Eventually, the heart may fail to pump with as much force as needed.
Uncontrolled high blood pressure is the most common cause of left ventricular hypertrophy. Complications include irregular heart rhythms, called arrhythmias, and heart failure.
Treatment of left ventricular hypertrophy depends on the cause. Treatment may include medications or surgery.
Symptoms
Left ventricular hypertrophy usually develops gradually. Some people do not have symptoms, especially during the early stages of the condition.
Left ventricular hypertrophy itself doesn't cause symptoms. But symptoms may occur as the strain on the heart worsens. They may include:
- Shortness of breath, especially while lying down.
- Swelling of the legs.
- Chest pain, often when exercising.
- Sensation of rapid, fluttering or pounding heartbeats, called palpitations.
- Fainting or a feeling of lightheadedness.
When to see a doctor
Seek emergency care if:
- You feel chest pain that lasts more than a few minutes.
- You have severe difficulty breathing.
- You have severe lightheadedness or lose consciousness.
- You have a sudden, severe headache, difficulty speaking, or weakness on one side of your body.
If you have mild shortness of breath or other symptoms, such as palpitations, see your healthcare professional.
If you have high blood pressure or another condition that increases the risk of left ventricular hypertrophy, your healthcare team is likely to recommend regular health checkups to check your heart.
Causes
Anything that puts stress on the heart's lower left chamber can cause left ventricular hypertrophy. The lower left chamber is called the left ventricle. As the strain on the lower left chamber increases, the muscle tissue in the chamber wall thickens. Sometimes, the size of the heart chamber itself also increases.
Left ventricular hypertrophy also may be caused by gene changes that affect the heart muscle's structure.
Things that can cause the heart to work harder and may possibly lead to left ventricular hypertrophy include:
- High blood pressure. Also called hypertension, this is the most common cause of left ventricular hypertrophy. Long-term high blood pressure strains the left side of the heart, causing it to grow bigger. Treating high blood pressure can help reduce left ventricular hypertrophy symptoms and may even reverse it.
- Narrowing of the aortic valve. The aortic valve is between the lower left heart chamber and the body's main artery, called the aorta. Narrowing of the valve is called aortic stenosis. When the valve is narrowed, the heart must work harder to pump blood into the aorta.
- Intensive athletic training. Intense, long-term strength and endurance training causes changes in the heart. The changes help the heart handle the extra physical workload. But the changes can make the heart muscle grow larger. Sometimes this is called athlete's heart or athletic heart syndrome. It's unclear whether the increased heart size in athletes can lead to stiffening of the heart muscle and disease.
Certain conditions passed down through families, called genetic conditions, can make the heart thicker. They include:
- Hypertrophic cardiomyopathy. This condition is caused by changes in genes that cause the heart muscle to thicken. The thickening makes it harder for the heart to pump blood. It can occur even without high blood pressure. People with one parent with hypertrophic cardiomyopathy have a 50% chance of having the changed gene that causes the disease.
- Amyloidosis. Proteins build up around the organs, including the heart. The collection of proteins interferes with how the organs work. When the condition is passed down through families, it is called familial amyloidosis. It also may affect the nerves and kidneys.
Risk factors
Things that increase the risk of left ventricular hypertrophy include:
- Age. Left ventricular hypertrophy is more common in older people. So is high blood pressure, which can cause heart muscle thickening.
- Weight. Being overweight increases the risk of high blood pressure and left ventricular hypertrophy.
- Family history. Changes in genes passed down through families may lead to left ventricular hypertrophy.
- Diabetes. Having diabetes increases the risk of left ventricular hypertrophy.
- Female gender. Women with high blood pressure are more likely to get the condition than are men with similar blood pressure measurements.
Complications
Left ventricular hypertrophy changes the structure of the heart and how the heart works. The thickened left ventricle becomes weak and stiff. This prevents the lower left heart chamber from filling properly with blood. As a result, blood pressure in the heart increases.
Complications of left ventricular hypertrophy include:
- Heart failure.
- Irregular heart rhythms, called arrhythmias.
- Too little oxygen to the heart, called ischemic heart disease.
- Sudden, unexpected loss of heart function, breathing and consciousness, called sudden cardiac arrest.
Prevention
The same healthy lifestyle changes recommended to treat high blood pressure also help prevent left ventricular hypertrophy. Try these tips:
- Don't smoke.
- Eat healthy foods.
- Use less salt.
- Limit or avoid alcohol.
- Get regular exercise.
- Maintain a healthy weight.
- Get 7 to 9 hours of sleep daily.
- Manage stress.
Uncontrolled high blood pressure increases the risk of left ventricular hypertrophy. Get your blood pressure checked at least every two years if you're 18 and older. If you have risk factors for heart disease or are over age 40, you may need more-frequent checks. Ask your healthcare team what blood pressure reading is best for you. Your healthcare professional may recommend checking your blood pressure at home. Home blood pressure monitors are available at local stores and pharmacies.
Diagnosis
To diagnose left ventricular hypertrophy, a healthcare professional does a physical exam and asks questions about your symptoms and family's health history. The care professional checks your blood pressure and listens to your heart with a device called a stethoscope.
Tests
Tests used to diagnose left ventricular hypertrophy may include:
- Lab tests. Blood and urine tests may be done to check for conditions that affect heart health. Tests may be done to check blood sugar, cholesterol levels, and liver and kidney function.
- Electrocardiogram. Also called an ECG or EKG, this quick and painless test measures the electrical activity of the heart. During an ECG, sensors called electrodes are attached to the chest and sometimes to the arms or legs. Wires connect the sensors to a machine, which displays or prints results. An ECG can show how well the heart is beating. Your care provider can look for signal patterns that suggest thickened heart muscle tissue.
- Echocardiogram. An echocardiogram uses sound waves to create pictures of the heart in motion. This test shows blood flow through the heart and heart valves. It can show thickened heart muscle tissue and heart valve problems related to left ventricular hypertrophy.
- Heart MRI. This test, also called a cardiac MRI, uses magnetic fields and radio waves to create detailed images of the heart.
Treatment
Treatment for left ventricular hypertrophy depends on the cause. It may include medicines, catheter procedures or surgery. It's important to manage conditions such as high blood pressure and sleep apnea, which can cause blood pressure to be higher.
Medications
Medicines are used to treat symptoms and prevent complications of left ventricular hypertrophy. Blood pressure medicines may help reduce or prevent thickening of the heart muscle. The type of medicine used depends on the cause of left ventricular hypertrophy.
Medicines that might be used to treat left ventricular hypertrophy or the conditions that cause it include:
- Angiotensin-converting enzyme inhibitors. Also called ACE inhibitors, these medicines widen blood vessels to lower blood pressure. They can improve blood flow and decrease the strain on the heart. Side effects include a persistent cough.
- Angiotensin II receptor blockers. Also called ARBs, these medicines have benefits similar to ACE inhibitors but don't cause a persistent cough.
- Beta blockers. These medicines help control the heart rate. They also help the heart move blood with less force.
- Calcium channel blockers. These medicines relax the heart muscle and widen blood vessels. This reduces blood pressure.
- Water pills, also called diuretics. These medicines reduce the amount of fluid in the body, lowering blood pressure.
Surgery or other procedures
Left ventricular hypertrophy that is caused by aortic valve stenosis might require a catheter procedure or surgery to repair or replace the valve.
Surgery or other procedures may be needed to treat underlying conditions such as:
- Hypertrophic cardiomyopathy. Surgery may be done if the condition causes heart failure symptoms or a blockage that interferes with the heart's pumping action.
- Amyloidosis. If other treatments don't work, a stem cell transplant may be needed. Treatment for amyloidosis is available at specialized clinics.
Together you and your care team can develop a treatment plan that's best for you.
Lifestyle and home remedies
Lifestyle changes can help lower blood pressure and improve heart health. Try these healthy lifestyle changes:
- Eat a nutritous, healthy diet. Choose fruits, vegetables, whole grains, low-fat dairy products and good fats, such as olive oil. Limit foods and beverages higher in added sugars, salt and saturated fat. Choose low-sodium or no-salt-added foods. Don't add salt to your meals.
- Don't smoke or use tobacco. Quitting is the best way to reduce the risk of heart disease and its complications. If you need help quitting, talk to your healthcare team.
- Limit or avoid alcohol. Alcohol can raise blood pressure, especially if consumed in large amounts. If you choose to drink alcohol, do so in moderation. For healthy adults, that means up to one drink a day for women and up to two drinks a day for men.
- Exercise regularly. Regular physical activity helps to lower blood pressure. With your healthcare team's OK, aim for at least 30 minutes of physical activity most days of the week. Some sports or exercises can temporarily raise blood pressure. Talk to your care team about the amount and type of exercise that's best for you.
- Manage weight. If you are overweight or have obesity, losing just a few pounds can help lower blood pressure. Weight loss may help reverse left ventricular hypertrophy. Talk with your healthcare team to set realistic goals for weight.
- Manage stress. Find ways to help reduce emotional stress. Getting more exercise, practicing mindfulness and connecting with others in support groups are some ways to reduce stress.
Preparing for an appointment
You may be referred to a doctor trained in treating heart diseases. This type of healthcare professional is called a cardiologist.
What you can do
- Write down your symptoms, including any that may seem unrelated to the reason you scheduled the appointment.
- Make a list of all your medicines, vitamins and supplements. Include the dosages.
- Write down important medical information, including other conditions you may have.
- Write down important personal information, including any recent life changes or stressors in your life.
- Write down questions to ask your healthcare team.
- Find out if your family has a history of heart disease.
- Ask someone to come with you to help you remember what the care provider says.
Questions to ask your doctor
- What's the most likely cause of my symptoms?
- What tests do I need? How do I prepare for them?
- What types of treatments do I need?
- Should I make any lifestyle changes?
- Should I restrict any of my activities?
- I have other health problems. How can I best manage these conditions together?
Don't hesitate to ask any other questions during your appointment.
What to expect from your doctor
Your healthcare professional is likely to ask you many questions. Being ready to answer them may leave time to go over items you want to spend more time on. You may be asked:
- What are your symptoms?
- When did the symptoms start?
- Have your symptoms gotten worse over time?
- Do you have chest pain or rapid, fluttering or pounding heartbeats?
- Do you have dizziness? Have you ever fainted?
- Have you had trouble breathing?
- Does exercise or lying down make your symptoms worse?
- Have you ever coughed up blood?
- Do you have a history of high blood pressure or rheumatic fever?
- Do you have a family history of heart problems?
- Do you or did you smoke?
- Do you use alcohol or caffeine?
© 1998-2026 Mayo Foundation for Medical Education and Research(MFMER). All rights reserved. Terms of Use
