Ruptured eardrum (perforated eardrum)
Conditions
Overview
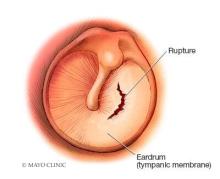
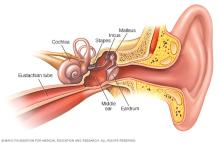
A ruptured eardrum, also called tympanic membrane perforation, is a hole or tear in the thin tissue, also called the eardrum, between the ear canal and the middle ear.
A ruptured eardrum can cause hearing loss. It also can make middle ear infections more likely.
A ruptured eardrum most often heals in a few weeks without treatment. But it might need a patch or surgical repair to heal.
Symptoms
Symptoms of a ruptured eardrum may include:
- Ear pain that may go away fast.
- Mucus, pus-filled liquids or bloody liquids coming out of the ear.
- Hearing loss.
- Ringing in the ear, also called tinnitus.
- Feeling of spinning, also called vertigo.
- Nausea or vomiting that can come from vertigo.
When to see a doctor
Make a medical appointment if you have symptoms of a ruptured eardrum.
Causes
Causes of a ruptured, also called perforated, eardrum may include:
- Middle ear infection, also called otitis media. A middle ear infection often occurs because of a buildup of fluids in the middle ear. Pressure from these fluids can cause the eardrum to rupture.
-
Barotrauma. Barotrauma is stress on the eardrum when the air pressure in the middle ear and the air pressure outside the ear are out of balance. If the pressure is bad enough, the eardrum can tear. Barotrauma is most often caused by air pressure changes during air travel.
Other things that can cause sudden changes in pressure and possibly a ruptured eardrum include scuba diving and something hitting the ear hard, such as an automobile air bag.
- Loud sounds or blasts, also called acoustic trauma. Loud sounds, such as from an explosion or gunshot, rarely can cause a tear in the eardrum.
- Putting things in the ear. Small objects, such as a cotton swab or hairpin, can poke through or tear the eardrum.
- Severe head trauma. Severe injury, such as a skull base fracture, may damage the middle and inner ears, including the eardrums.
Risk factors
Many factors can raise the risk of a ruptured eardrum, including:
- A middle ear infection.
- Airplane travel.
- Scuba diving.
- Severe head injury such as a skull base fracture.
- Putting things in the ear.
- A blow to the ear.
- Loud sounds or blasts.
Complications
The eardrum, also called tympanic membrane, has two main roles:
- Hearing. When sound waves strike it, the eardrum moves. This is the first step by which structures of the middle and inner ears translate sound waves into nerve impulses.
- Protection. The eardrum also acts as a barrier, protecting the middle ear from water, bacteria and other things that don't belong there.
If the eardrum ruptures, problems can happen, especially if it doesn't heal after 3 to 6 months. Complications aren't common. They include:
- Hearing loss. Usually, hearing loss is short-term, lasting only until the eardrum heals. Where the tear is and how big it is play a role in how much hearing is lost.
- Middle ear infection, also called otitis media. A ruptured eardrum can let bacteria into the ear. A small number of people might get repeated or ongoing, called chronic, infections if the hole doesn't heal. This small group might have ongoing fluid leaks from the ear and hearing loss.
-
Middle ear cyst, called cholesteatoma. Although rare, an eardrum rupture that doesn't heal can form this cyst in the middle ear. This cyst is made up of skin cells and other debris.
Ear canal debris often travels to the outer ear with the help of earwax. Earwax protects the ear. If the eardrum is torn, the skin debris can pass into the middle ear and form a cyst.
A cyst in the middle ear lets bacteria grow. And it has proteins that can damage the bones of the middle ear.
Prevention
Follow these tips to avoid a ruptured eardrum:
- Get treatment for middle ear infections. Be aware of the symptoms of middle ear infection. They include earache, fever, stuffy nose and not hearing as well. Children with middle ear infections often are fussy and may refuse to eat. Seek medical care right away to prevent damage to the eardrum.
-
Protect your ears while on airplanes. If possible, don't fly with a cold or an allergy that causes nose or ears to be stuffed up. During takeoffs and landings, keep ears clear with pressure-equalizing earplugs, yawning or chewing gum.
Or use the Valsalva maneuver — gently pushing air into the nose, as if blowing your nose, while pinching the nostrils and keeping the mouth closed. Don't sleep while the plane is taking off or landing.
- Keep things out of the ears. Don't use a cotton swab, paper clip or hairpin to dig out earwax. These can tear the eardrum. Teach children about the damage they can do by putting things in their ears.
- Guard against loud noise. Stay away from loud noises. If you have to be around loud noises, such as at work, wear earplugs or earmuffs.
Diagnosis
A healthcare professional or an ENT specialist often can see a ruptured eardrum by looking inside the ear with a tool that has a light, called an otoscope.
Other tests might help your healthcare professional find the cause of the ear symptoms or see if there's hearing loss. These tests include:
- Lab tests. For fluid from the ear, a lab test might find a bacterial infection of the middle ear.
-
Tuning fork test. Tuning forks are metal tools that make sounds when struck. Simple tests with tuning forks can help find hearing loss.
A tuning fork test also might show the cause of hearing loss. The cause might be damage to the moving parts of the middle ear, including the eardrum; damage to sensors or nerves of the inner ear; or damage to both.
- Tympanometry. A tool put into the ear canal measures how the eardrum reacts to small changes in air pressure. This can show whether an eardrum is torn.
- Audiology exam. This is a series of tests done in a soundproof booth. They measure hearing at different volumes and pitches.
Treatment
Most ruptured eardrums heal without treatment within a few weeks. Antibiotic drops can treat an infection. If the hole doesn't heal by itself, treatment might involve ways to close the hole. These may include:
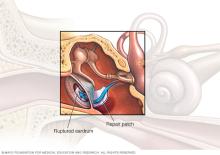
-
Eardrum patch. An ENT specialist might seal the hole with a patch made of paper or something else.
This procedure is done in an office. It involves putting a chemical on the edges of the tear. This can help the eardrum heal. A patch is put over the hole. This might need to be done more than once before the hole closes.
-
Surgery. This might be the next step if a patch won't or can't fix the tear.
The most common surgery is called tympanoplasty. Your surgeon makes a patch of your own tissue to close the hole in the eardrum. This procedure is done on an outpatient basis. You're likely to go home the same day.
Self care
A ruptured eardrum usually heals on its own within weeks. Sometimes, healing takes months. Until your healthcare professional tells you that your ear is healed, protect it by:
- Keeping the ear dry. Put a waterproof earplug made of silicone or a cotton ball coated with petroleum jelly in the ear when showering or bathing.
- Don't clean the ears. Give the eardrum time to heal all the way.
- Don't blow the nose. Nose blowing can cause pressure that can damage the healing eardrum.
Preparing for your appointment
If you have symptoms of a ruptured eardrum, you're likely to start by seeing your healthcare professional. You may be referred to a specialist in ear, nose and throat (ENT) conditions.
Here's some information to help you get ready for your appointment.
What you can do
Make a list to share with your healthcare professional. Your list should include:
- Your symptoms, including any that don't seem to be related to your ears, and when they began.
- Things that may be related to your ear problems. These include a history of ear infections, recent ear injuries or head traumas, or recent air travel.
- All medicines, vitamins or supplements you take, including doses.
- Questions for your healthcare professional.
Basic questions about ruptured eardrums might include:
- Do I have a ruptured eardrum?
- What else could be causing my hearing loss and other symptoms?
- If I have a ruptured eardrum, what do I need to do to protect my ear while it's healing?
- What follow-up appointments will I need?
- When do we need to consider other treatments?
Be sure to ask all the questions you have about your ears.
What to expect from your doctor
Your healthcare professional is likely to ask you a number of questions, including:
- Did you have symptoms such as pain or feeling like you're spinning that cleared up?
- Have you had ear infections?
- Have you been around loud sounds?
- Have you been swimming or diving recently?
- Have you recently flown?
- Have you had head injuries?
- Do you put anything in your ear to clean it?
What you can do in the meantime
If you think that you have a ruptured eardrum, try to prevent infection by keeping your ears dry.
Don't swim until your healthcare professional says it's OK. To keep water out of the ear when showering or bathing, use a waterproof earplug you can mold or put a cotton ball coated with petroleum jelly in the outer ear.
Don't put medicine drops in the ear unless your healthcare professional prescribes them for an infection related to the perforated eardrum.
© 1998-2026 Mayo Foundation for Medical Education and Research(MFMER). All rights reserved. Terms of Use
