Vulvodynia
Conditions
Overview
Vulvodynia (vul-voe-DIN-e-uh) is a type of long-term pain or discomfort around the outer part of the female genitals, called the vulva. It lasts at least three months and has no clear cause. The pain, burning or irritation linked with vulvodynia can make you so uncomfortable that sitting for a long time or having sex becomes unthinkable. The condition can last for months to years.
If you have symptoms of vulvodynia, don't let embarrassment or a lack of visible signs stop you from talking with your gynecologist or another healthcare professional. Treatments can ease your discomfort. And your care team might be able to find a cause for your pain. So, it's key to get a medical exam.
Symptoms
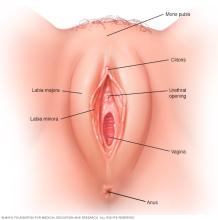
The main vulvodynia symptom is pain in the vulva, which includes the opening of the vagina. The pain often is described as:
- Burning.
- Irritation.
- Stinging.
- Rawness.
- Soreness.
- Sharp or knife-like pain.
You also may feel aching, throbbing and swelling.
How often the symptoms happen and where exactly they're felt varies from person to person. Your pain might be constant, or it may come and go. It might flare up only when the vulva is touched. You might feel the pain throughout your entire vulva. This is called generalized vulvodynia. Or the pain may flare up in a certain area, such as the tissue surrounding the opening of the vagina, called the vestibule. This is known as localized vulvodynia, and it's more common than the generalized kind.
The tissue of the vulva might look slightly inflamed or swollen. More often, your vulva doesn't look different than usual.
When to see a doctor
If you have pain in your vulva, talk with your gynecologist or another member of your healthcare team. If you don't have a gynecologist, you might be referred to one. A healthcare professional needs to find out if your pain has a treatable cause that's different from vulvodynia, such as:
- An active infection from yeast or bacteria.
- A sexually transmitted disease such as herpes.
- An inflammatory skin condition.
- Vulvar growths.
- Genitourinary syndrome of menopause.
Some people who don't realize they have vulvodynia try to ease their symptoms by using yeast infection treatments without a prescription. But it's key to get a checkup, so a member of your healthcare team can give you an exam and recommend the right treatment for you.
Causes
Experts don't know what causes vulvodynia. Factors that might play a role include:
- Injury to or irritation of the nerves of the vulva.
- Past infections of the vagina.
- Painful swelling called inflammation that affects the vulva.
- Some genetic conditions.
- Allergies.
- Hormonal changes.
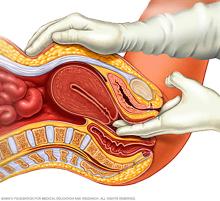
- Muscle spasm or weakness in the pelvic floor, which supports the uterus, bladder and bowel.
Complications
Without treatment, vulvodynia can affect mental health, relationships and other aspects of your life.
The condition is linked with anxiety and depression. It's also tied to less sexual desire, arousal and enjoyment. Fear of having painful sex can cause spasms in the muscles around the vagina, a condition called vaginismus. Intimacy issues such as these lead many people with vulvodynia to say they feel shame, lower self-esteem, negative about body image and lacking as a sexual partner.
The pain and other symptoms of vulvodynia might make it harder to keep up with work. You may feel less social too. And you may have trouble getting quality sleep.
Diagnosis
With vulvodynia, your gynecologist or another member of your care team likely will ask you questions about your medical and sexual history. You'll also be asked if you've had any surgeries.
You also might have a:
- Pelvic exam. Your outer genitals and vagina are checked for signs of an infection or other causes of your symptoms. A sample of cells from your vagina might be taken to test for an infection caused by yeast or bacteria. Your health care professional also might insert a gloved finger into your vagina to check the pelvic floor muscles for tenderness.
- Cotton swab test. A moistened cotton swab is used to gently check for specific areas of pain in your vulva. If a painful area is found, you'll likely be asked what it feels like and how much it hurts.
- Biopsy. If the skin of the vulva looks different than usual, your doctor or gynecologist might remove a small sample of tissue for a lab to check.
- Blood test. This may be done to check your levels of hormones such as estrogen, progesterone and testosterone.
Treatment
Vulvodynia treatments focus on relieving symptoms. No one treatment works in every case. For many people, a mix of treatments works best. It can take time to find the right combination. It also can take months to get relief.
Medications
Your health care team may recommend medicines such as:
- Antidepressants or anticonvulsants. These can help ease long-term pain. Some types of antidepressants come in the form of creams that can be put on the skin.
- Local anesthetics. These stronger medicines can block pain for a short time. For example, you might put a local anesthetic called lidocaine ointment on your vulva 30 minutes before you have sex to make it more comfortable. This medicine can cause your partner to lose feeling for a little while after sexual contact.
- Nerve blocks. These shots are given near a nerve or group of nerves that are sensitive to pain. These might help if you have long-standing pain that doesn't respond to other treatments.
- Hormone creams. If your symptoms are linked to hormonal changes, you might get relief from estrogen cream that goes into your vagina. Sometimes it's prescribed along with testosterone cream.
- Antihistamines. Often used to treat allergies, these medicines also might reduce itching from vulvodynia. But antihistamines may be drying if you are past menopause.
Therapies
Physical therapy includes various techniques that may ease your pain and improve your quality of life. These include:
Pelvic floor therapy. Many people with vulvodynia have tension in the muscles of the pelvic floor, which supports the uterus, bladder and bowel. Exercises to stretch and relax those muscles can help ease vulvodynia pain.
Your physical therapist also might recommend that you use a device at home called a vaginal dilator. This stretches and stimulates the vagina. It also may help ease the fear of having pain during sex.
- Biofeedback. This mind-body technique can help relieve pain by teaching you how to relax your pelvic muscles. It also can teach you to control how your body responds to the symptoms.
Talk therapy involves working with a therapist, who can teach you ways to cope with your pain. Examples include:
Cognitive behavioral therapy. This technique helps you notice negative thoughts and respond in practical ways. You'll also likely be encouraged to keep a daily pain diary. In the diary, you note when you have vulvodynia symptoms and what seems to make them better or worse.
Sometimes, vulvodynia pain might be linked with conflict in a relationship or with past trauma. Therapy can help people work through these challenges as well.
- Couples therapy or sex therapy. A therapist can teach you and your partner how to communicate better and build intimacy in ways that take the focus off sex. You also might learn how to relieve the fear of pain during sex.
Surgery or other procedures
Surgery may be a treatment choice if you have pain in the tissue that surrounds the opening of your vagina, called the vestibule. Most often, surgery is done only if other treatments haven't helped.
Surgery can remove the painful vestibule tissue from the vulva. The procedure is called a vestibulectomy. If you have vulvodynia symptoms in other parts of your vulva, surgery likely isn't a treatment option for you.
If you're thinking about getting this operation, ask your health care team to explain all of the benefits and risks. Sometimes, surgery can lead to scarring or worse pain.
Alternative medicine
Some treatments that aren't part of standard medical care may help lessen vulvodynia symptoms. These include:
- Acupuncture. A trained practitioner places very fine needles into specific parts of the body.
- Hypnosis. A health professional guides you into a changed state of awareness that may help you relax and focus.
- Mindfulness and meditation. You can learn these techniques through self-instruction with practice and with apps.
- Transcutaneous electrical nerve stimulation. A device placed on the skin sends low-voltage electrical currents to the painful area.
Stress tends to make vulvodynia worse. And having vulvodynia can cause you to have more stress. Activities that can help ease stress include yoga and mindfulness mediation.
Lifestyle and home remedies
Simple self-care steps may help you manage vulvodynia symptoms.
Some tips for work are:
- Get comfortable. If you sit a lot during the day, use a foam rubber-donut cushion.
- Try to stand more. This takes pressure off the areas around your vulva.
Tips for exercise include:
- Limit high-intensity exercises, such as running. These create friction that can irritate the vulva.
- Use a frozen gel pack after exercise. Wrap it in a towel and put in on your vulva for up to 15 minutes to ease any symptoms.
- Limit activities that put pressure on your vulva, such as biking or horseback riding.
Tips for bathing and swimming include:
- Wash gently. Scrubbing the affected area harshly or washing too often can make irritation worse. Instead, use plain lukewarm or cool water to gently clean your vulva with your hand. Then pat the area dry. After you bathe, put on a preservative-free emollient, such as plain petroleum jelly. This creates a protective barrier.
- Stay away from products that can irritate the vulva. Don't use bubble bath, feminine hygiene products, or perfumed creams or soaps.
- Soak in a sitz bath. Two to three times a day, sit in lukewarm or cool water with Epsom salts or colloidal oatmeal for 5 to 10 minutes. This may help relieve burning and irritation.
- Stay out of hot tubs and hot baths. Spending time in hot water can cause discomfort and itching.
- Swim in pools that don't have a lot of chlorine. This pool disinfectant keeps the water clean, but too much can be irritating.
Some hygiene tips are:
- Don't use deodorant tampons or pads. The deodorant can be irritating. Instead, use pads and tampons that are 100% cotton.
- Use toilet paper that is soft, white and unscented.
- Urinate before your bladder feels full. Then rinse your vulva with water and pat dry.
Some tips for clothing and laundry are:
- Wear loose-fitting clothes. Tight clothing limits airflow to your vulva, which can be irritating to the area. Wear 100% cotton underwear instead of nylon underwear. Try sleeping without underwear at night. Also make sure to wear loose pants and skirts. Choose thigh-high or knee-high hose instead of pantyhose.
- After a workout, take off exercise clothes right away. Remove a wet bathing suit after you swim too.
- Use laundry detergents made for sensitive skin. And don't use fabric softener on underwear.
- If your washing machine has a double- or extra-rinse cycle, use it on clothes that come in contact with your vulva. This helps rinse off detergent.
If you're sexually active:
- Use a water-based lubricant. Put it on before you have sex. Don't use products that contain alcohol, dyes, perfume, flavor, or warming or cooling ingredients.
- Choose your birth control with care. Keep in mind that spermicide or contraceptive creams may be irritating. Talk with your doctor or other member of your care team about a form of birth control that won't irritate your vulva.
- Urinate after sex. This can lower your chances of getting an infection. After you urinate, rinse your vulva with cool water and pat dry.
- Try cold compresses or gel packs to ease burning. Wrap them in a towel and place them on your vulva for 15 minutes at a time.
Coping and support
You might find it helpful to talk with other people who have vulvodynia. You can share information, talk about your experiences and feel less alone. If you don't want to join a support group, a member of your care team might be able to recommend a counselor in your area who has experience helping people with vulvodynia.
Preparing for an appointment
You're likely to start by seeing your primary care doctor. In some cases, you may be referred to a doctor who specializes in conditions of the female reproductive tract, called a gynecologist.
What you can do
Make a list of:
- Your symptoms, including any that may not seem related to the reason for which you scheduled the appointment. Note when the symptoms began.
- Your medical history, including other conditions for which you're being treated.
- All medicines, vitamins or other supplements you take, including the amounts you take, called doses.
- Questions to ask your care team.
For vulvodynia, questions to ask your care team include:
- What could be causing my symptoms?
- What tests do you recommend?
- What treatments are most likely to improve my symptoms?
- When might I expect to get relief?
- I have other medical conditions. How can I manage them together?
- Do you have brochures or other printed material I can have? What websites do you recommend?
Feel free to ask other questions during your appointment too — especially if you need more information or you don't understand something.
What to expect from your doctor
You may be asked several questions, such as:
- How bad is your pain, and how long does it last? How would you describe it?
- Is your pain often triggered by a specific event, such as sex, exercise or going to the bathroom?
- Does your menstrual cycle affect your pain?
- Does anything make your pain better or worse?
- Have you had pelvic surgery?
- Have you been pregnant or could you be pregnant now?
- Have you been treated for urinary tract or vaginal infections?
© 1998-2026 Mayo Foundation for Medical Education and Research(MFMER). All rights reserved. Terms of Use
