Septoplasty
Procedures
Overview
Septoplasty (SEP-toe-plas-tee) is a type of nose surgery. It straightens the wall of bone and cartilage that divides the space between the two nostrils. That wall is called the septum. When the septum is crooked, it's known as a deviated septum. A deviated septum can make it harder to breathe through the nose.
During septoplasty, the septum is moved back to the middle of the nose. To do this, the surgeon may need to cut and remove parts of the septum first. Then, these parts might be placed back into the nose in a corrected position.
Once you've healed from a septoplasty, you'll likely find it's easier to breathe. But before you get this surgery, talk with a surgeon about what results to expect.
Why it's done
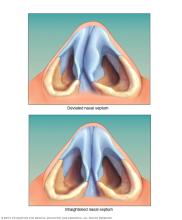
A crooked septum is common. But when it's very crooked, a deviated septum can block one side of the nose and reduce airflow. This makes it hard to breathe through one or both sides of your nose.
Septoplasty straightens the nasal septum. The surgeon does this by trimming, moving and replacing cartilage, bone or both.
Surgery to fix a deviated septum might be right for you if your symptoms affect your quality of life. For example, you might have trouble breathing through your nose or have frequent nosebleeds.
Risks
As with any major surgery, septoplasty carries risks. These risks include bleeding, infection and a bad reaction to the medicine that keeps you from feeling pain during surgery, called anesthesia.
Other risks specific to septoplasty include:
- Continued symptoms, such as blocked air flow through the nose.
- Serious bleeding.
- A change in the shape of the nose.
- A hole in the septum.
- Less sense of smell.
- Clotted blood in the nasal space that has to be drained.
- Short-term loss of feeling in the upper gum, teeth or nose.
- Poor-healing surgical cuts, also called incisions.
You may need more surgery to treat some of these health issues. You also may need more surgery if you didn't get the results you expected from septoplasty. Talk with your surgeon about your specific risks before surgery.
How you prepare
Before you schedule a septoplasty, you'll likely meet with a surgeon. The surgeon talks with you about the benefits and risks of the surgery. This meeting may include:
- Review of your medical history. Your surgeon asks about conditions you have or have had in the past. You're also asked if you take any medicines or supplements.
- A physical exam. The surgeon checks your skin and the inside and outside of your nose. You also may be asked to get certain tests, such as blood tests.
- Photographs. Someone from the surgeon's office may take photos of your nose from different angles. If the surgeon thinks that septoplasty will change the outside of your nose, the surgeon can use these photos to talk with you about it. The photos also can be used for the surgeon's reference during and after surgery.
- A talk about your goals. You and your surgeon should talk about what you hope to gain from surgery. The surgeon likely will explain what septoplasty can and can't do for you, and what your results might be.
Food and medications
Don't take medicines that contain aspirin or ibuprofen (Advil, Motrin IB, others) before and after surgery. They may increase bleeding. Take only medicines approved or prescribed by your surgeon.
Other safety measures
If you smoke, stop smoking. Smoking raises your risk of having problems during and after surgery. It can slow the healing process too.
What you can expect
Septoplasty straightens the nasal septum. It does this by trimming, centering, and sometimes replacing cartilage or bone. The surgeon works through incisions inside the nose. Sometimes, a small incision between the nostrils needs to be made.
If crooked nasal bones push the septum off to one side, the surgeon may need to make cuts in the bones of the nose. This is done to move them into their proper place. Small strips of cartilage called spreader grafts can help correct a deviated septum when the problem is along the bridge of the nose. Sometimes, these are used to help straighten the septum.
During the procedure
The surgery is done with medicine to keep you from feeling pain, called anesthesia. The type of anesthesia used depends on how complex your surgery is and what you and your surgeon prefer.
- Local anesthesia. This type of anesthesia is limited to your nose. Your doctor injects the pain-numbing medicine into your nasal tissues. If you'll also be sedated, that is done using medicine through a needle in a vein. The medicine makes you groggy but doesn't put you in a sleep-like state.
- General anesthesia. This is medicine that you breathe in or receive through a needle in a vein. General anesthesia affects your entire body and puts you in a sleep-like state.
Talk with your surgeon before surgery about which kind of anesthesia is best for you.
The incisions are closed with sutures that dissolve on their own over time. Soft silicone splints may be placed inside each nostril to support the septum. To prevent bleeding after surgery, your care team may place bandage-like material called packing in your nose.
After surgery, you're moved to a recovery room. The staff closely watches you. Most often, septoplasty is done on an outpatient basis. That means you'll likely be able to go home the same day. You'll need someone to drive you home.
After the procedure
To lower the chances of bleeding and swelling, your surgeon may have you follow some safety steps for a few weeks. Depending on the extent of your surgery, you may not need to do all of the following:
- Sleep on your back with your head elevated.
- Don't blow your nose for at least a few weeks.
- Wear clothes that fasten in the front. Do not pull clothing, such as shirts or sweaters, over your head.
- Stay away from heavy lifting and strenuous activities, such as aerobics and jogging, for up to six weeks. This lowers the chances of a nosebleed.
Your surgeon prescribes medicine to ease pain.
Results
By 3 to 6 months after surgery, the tissues in your nose likely will be somewhat stable. It's still possible that cartilage and tissue may move or change shape over time. Some changes can happen for up to a year or more after surgery.
Many people find that septoplasty improves symptoms that were caused by a deviated septum, such as trouble breathing. But the results vary by person.
Some people find that their symptoms continue after surgery. They might choose to get a second septoplasty to further refine the nose and septum.
© 1998-2026 Mayo Foundation for Medical Education and Research(MFMER). All rights reserved. Terms of Use
